Acid reflux, also known as heartburn, is a common digestive issue experienced by millions worldwide. It occurs when stomach acid flows back up into the esophagus—the tube connecting your mouth to your stomach—causing irritation and discomfort. While many associate it with specific foods or dietary habits, a significant number of people notice their symptoms flare up during periods of increased stress. This isn’t merely coincidental; there’s a complex interplay between our emotional state, nervous system, and digestive processes that explains why stressful times often exacerbate acid reflux. Understanding this connection can empower individuals to manage their symptoms more effectively and proactively address both the physical and psychological components contributing to their discomfort.
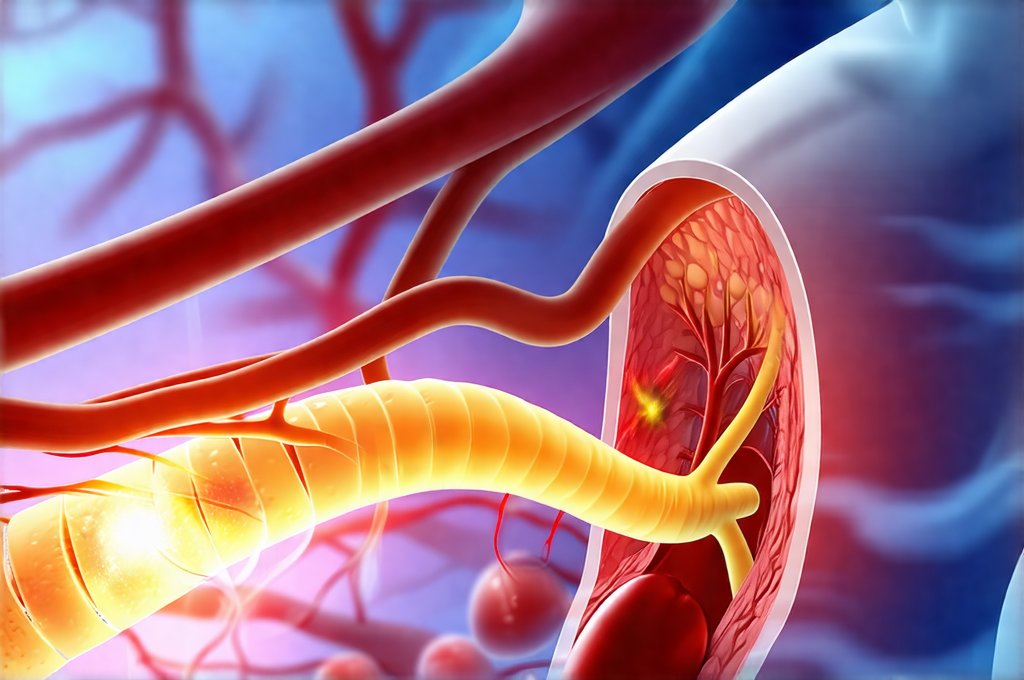
The gut is often referred to as the “second brain” for a reason. It possesses its own intricate nervous system, known as the enteric nervous system (ENS), which communicates extensively with the brain via what’s called the gut-brain axis. This bidirectional communication pathway means that our emotional state can profoundly impact digestive function, and conversely, problems in the gut can influence mood and mental wellbeing. Stress triggers a cascade of physiological responses designed to prepare us for “fight or flight,” diverting energy away from non-essential functions like digestion. When we’re chronically stressed, this disruption can lead to a variety of gastrointestinal issues, including increased acid production, delayed stomach emptying, and heightened sensitivity to discomfort – all factors that contribute to worsening acid reflux symptoms. Recognizing when gut trouble is worse can help you manage stress.
The Stress Response & Digestive Disruption
The body’s stress response is a survival mechanism evolved over millennia. When we perceive a threat—whether it’s a looming deadline at work or a challenging personal situation—the sympathetic nervous system kicks into gear. This triggers the release of hormones like cortisol and adrenaline. These hormones serve to:
– Increase heart rate and blood pressure, preparing us for action.
– Redirect blood flow away from digestive organs towards muscles and vital organs.
– Suppress digestion temporarily.
While beneficial in acute situations requiring immediate physical exertion, chronic activation of the stress response has detrimental effects on digestive health. Prolonged cortisol exposure can actually increase stomach acid production, making reflux more likely. Furthermore, stress often leads to changes in eating habits – many people turn to comfort foods high in fat or sugar when stressed, which are known triggers for acid reflux. This creates a vicious cycle where stress worsens digestion, and digestive discomfort adds to overall stress levels. Understanding hormonal shifts can help you manage symptoms.
Beyond hormonal shifts, stress can also impact the motility of the gastrointestinal tract. Motility refers to the movement of food through the digestive system. Stress tends to either speed up or slow down this process, neither of which is ideal for those prone to acid reflux. Rapid transit can lead to insufficient digestion and increased gas production, while delayed emptying increases pressure on the lower esophageal sphincter (LES) – the muscle that prevents stomach acid from flowing back into the esophagus. A weakened or improperly functioning LES is a primary cause of acid reflux.
How Stress Impacts the Lower Esophageal Sphincter (LES)
The LES acts as a gatekeeper, ensuring one-way traffic between the stomach and esophagus. Its proper function relies on several factors, including muscle tone and pressure. Chronic stress has been demonstrably linked to decreased LES tone. When the LES weakens, it’s easier for stomach acid to escape upwards. The mechanisms behind this aren’t fully understood, but research suggests a few possibilities:
- Cortisol can directly affect the muscles of the LES, reducing their ability to contract effectively.
- Stress-induced changes in breathing patterns (such as shallow or rapid breathing) can increase abdominal pressure, pushing stomach contents upward.
- Increased tension in the diaphragm and abdominal muscles, common responses to stress, can also contribute to higher intra-abdominal pressure.
It’s important to recognize that the LES isn’t always the sole culprit. Even with a normally functioning LES, increased acid production or delayed gastric emptying due to stress can overwhelm its capacity and lead to reflux symptoms. Addressing stress is therefore often crucial for managing acid reflux effectively. You may also wonder if acid reflux is linked to food sensitivities.
Stress & Visceral Hypersensitivity
Visceral hypersensitivity refers to an amplified perception of pain or discomfort originating from internal organs. People with visceral hypersensitivity experience more intense reactions to normal digestive processes, making them acutely aware of even minor sensations like gas or bloating. Stress can significantly exacerbate visceral hypersensitivity in several ways:
- It lowers the threshold for pain detection in the gut, meaning less stimulation is needed to trigger discomfort.
- It amplifies the brain’s interpretation of signals from the digestive system, leading to an overestimation of their severity.
- Chronic stress can alter the nervous system’s processing of visceral sensations, making individuals more sensitive to abdominal discomfort.
This heightened sensitivity means that even small amounts of acid reflux can feel intensely painful or bothersome in someone experiencing stress. It also contributes to a cycle of anxiety surrounding digestion – fearing heartburn can actually make it more likely to occur and feel worse when it does.
Lifestyle Adjustments for Stress & Acid Reflux
Managing the impact of stress on acid reflux requires a multifaceted approach. Focusing solely on dietary changes or medications often isn’t enough; addressing the underlying psychological factors is essential. Here are some strategies to consider:
- Stress Reduction Techniques: Incorporate regular practices like mindfulness meditation, deep breathing exercises, yoga, or tai chi into your routine. These techniques help calm the nervous system and reduce cortisol levels.
- Regular Exercise: Physical activity is a powerful stress reliever. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Prioritize Sleep: Adequate sleep is crucial for both physical and mental wellbeing. Establish a regular sleep schedule and create a relaxing bedtime routine.
- Time Management & Boundaries: Learn to prioritize tasks, delegate when possible, and set healthy boundaries to avoid overcommitment and chronic overwhelm.
- Seek Support: Don’t hesitate to reach out to friends, family, or a therapist for support if you’re struggling to manage stress on your own. Professional guidance can provide valuable tools and coping strategies. Stressful mornings may be a contributor.
The Vagus Nerve Connection
The vagus nerve is the longest cranial nerve in the body and plays a vital role in regulating numerous bodily functions, including digestion. It forms a critical link between the brain and the gut, transmitting signals in both directions as part of the gut-brain axis. Stress can disrupt vagal tone—the activity level of the vagus nerve—leading to impaired digestive function and increased susceptibility to acid reflux. Low vagal tone is associated with:
- Reduced gastric motility, leading to delayed stomach emptying.
- Impaired LES function, making it easier for acid to flow back into the esophagus.
- Increased inflammation in the gut.
Conversely, high vagal tone is linked to better digestive health, reduced stress reactivity, and improved overall wellbeing. Cultivating practices that enhance vagal tone can therefore be a powerful strategy for managing both stress and acid reflux symptoms. One key method is vagus nerve stimulation (VNS), but it doesn’t require expensive devices—simple techniques can often make a difference. It’s also important to consider if there is an enzyme deficiency.
The good news is that vagal tone isn’t fixed; it can be improved through conscious effort. Activities like singing, humming, gargling, and even cold water immersion have been shown to stimulate the vagus nerve and increase its activity. Focusing on slow, diaphragmatic breathing (belly breathing) also activates the vagus nerve and promotes relaxation. By incorporating these practices into your daily routine, you can help strengthen this crucial connection between brain and gut, leading to improved digestive health and reduced stress levels.
Ultimately, understanding the intricate relationship between stress and acid reflux is the first step towards effective management. It’s not simply about eliminating trigger foods or taking antacids; it’s about addressing the underlying psychological and physiological factors that contribute to your symptoms. By prioritizing stress reduction, lifestyle adjustments, and techniques to enhance vagal tone, you can regain control of your digestive health and improve your overall quality of life.