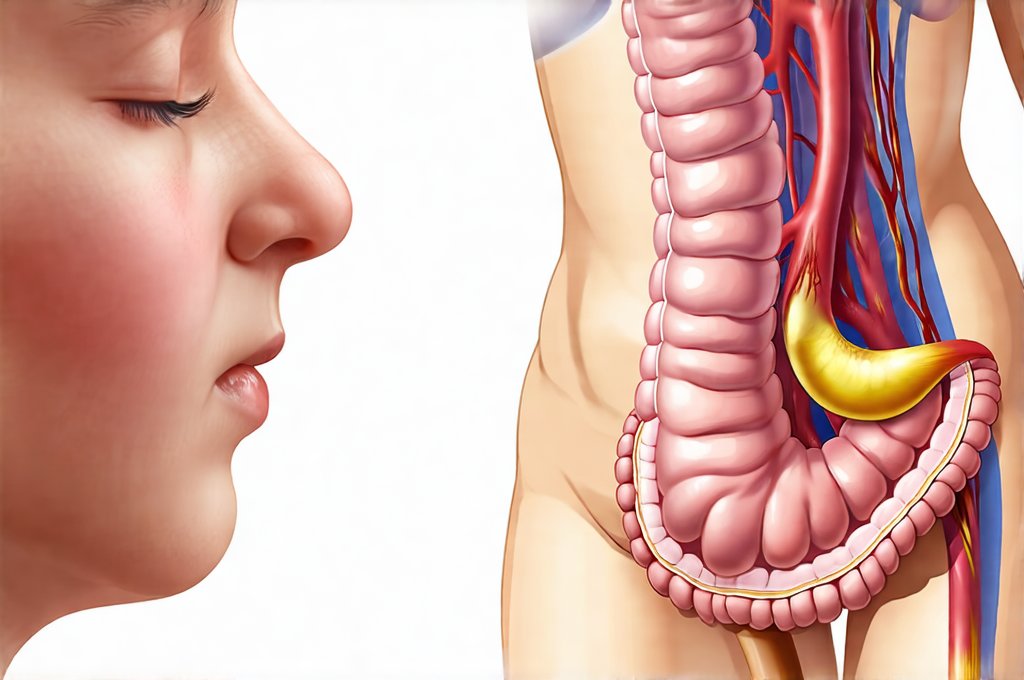
The gut microbiome – an intricate ecosystem residing within our digestive tract – is increasingly recognized as central to overall health. It’s no longer simply about digestion; this microbial community profoundly impacts immunity, mental wellbeing, hormone regulation, and even chronic disease risk. Traditional diagnostic methods often fall short in fully assessing the complexities of gut health. While standard tests might identify obvious issues like bacterial overgrowth or parasite infections, they rarely paint a complete picture of microbial diversity, functional capacity, or potential imbalances that could be contributing to systemic symptoms. This is where comprehensive stool testing, commonly referred to as a “gut panel,” comes into play – offering a much deeper dive into the workings of this critical internal environment.
The decision to pursue a full gut panel isn’t something to take lightly. It’s not a routine check-up like an annual physical. Instead, it’s typically recommended when conventional testing fails to explain persistent symptoms or when there is strong suspicion of underlying gut dysfunction. Understanding when to ask your doctor a gut panel is appropriate and what information it can provide empowers individuals to proactively address potential health concerns and work with healthcare professionals to develop targeted interventions. The goal isn’t just to identify “bad bugs,” but rather to understand the overall ecosystem, its functionality, and how it’s interacting with your body – ultimately paving the way for personalized strategies that support lasting wellbeing.
Recognizing the Signals: When to Consider a Gut Panel
Many conditions can have roots in gut health, making symptom recognition crucial. It’s important to note that these symptoms aren’t necessarily caused by gut issues but may be significantly influenced or exacerbated by them. A persistent pattern of digestive complaints is often the most obvious indicator, however, systemic and seemingly unrelated symptoms should also raise a flag. These include:
- Frequent bloating and gas
- Diarrhea, constipation, or alternating between both (IBS-like symptoms)
- Abdominal pain or cramping that doesn’t have an easily identifiable cause
- Heartburn or acid reflux that is resistant to typical treatments
- Undiagnosed food sensitivities or intolerances
- Skin conditions like eczema, psoriasis, or acne. The gut-skin axis is a well-established link, and imbalances can manifest in skin health.
- Autoimmune diseases: Growing research suggests the microbiome plays a role in autoimmune responses.
- Mood disorders such as anxiety and depression: The gut-brain axis highlights the bidirectional communication between the digestive system and the brain.
- Chronic fatigue or unexplained tiredness.
It’s also vital to consider lifestyle factors that can disrupt gut health, like prolonged antibiotic use, chronic stress, a diet high in processed foods and low in fiber, and environmental toxins. If you have a history of any of these factors and are experiencing the symptoms above, it’s worth discussing a gut panel with your healthcare provider. Don’t self-diagnose. A qualified practitioner can properly interpret results and guide appropriate interventions. If you feel you need to seek another opinion regarding your symptoms, consider a second opinion.
Understanding What Gut Panels Assess
A comprehensive stool test isn’t simply looking for pathogens. It provides an in-depth analysis of several key areas, allowing for a more nuanced understanding of gut health. These include:
- Microbial Diversity: This assesses the variety of bacterial species present. A diverse microbiome is generally considered healthier and more resilient.
- Specific Bacterial Populations: Identifying imbalances between beneficial and potentially harmful bacteria. It’s not about eliminating “bad” bacteria entirely, but rather restoring a healthy balance.
- Fungal Overgrowth: Detecting an overabundance of yeast or other fungi, which can disrupt the gut environment.
- Parasite Screening: Identifying parasitic infections that may be contributing to symptoms.
- Digestive Function Markers: Assessing levels of enzymes like elastase (indicating pancreatic function) and calprotectin (a marker of inflammation).
- Inflammation Markers: Determining if there’s evidence of chronic gut inflammation, which can contribute to various health issues.
- Short Chain Fatty Acid (SCFA) Analysis: SCFAs are produced by beneficial bacteria during fiber fermentation and play a crucial role in gut health and overall wellbeing.
The information gathered from a gut panel allows for personalized interventions such as dietary changes, probiotic supplementation, prebiotic foods, lifestyle modifications, or targeted therapies to address specific imbalances. It moves beyond generic recommendations and focuses on restoring the unique ecosystem within your gut. A more thorough understanding can be gained by combining multiple tests.
Deciphering Results: What to Expect
Once you’ve completed a stool collection (following specific instructions provided by the testing lab), the sample is sent for analysis. Results typically take 1-3 weeks to return, and are usually presented in a detailed report. However, raw data alone can be difficult to interpret without professional guidance. The key isn’t just what the results say but how they relate to your individual symptoms and health history.
A healthcare provider experienced in functional medicine or gut health will be able to translate the findings into actionable steps. They’ll look at the overall picture, considering microbial diversity, specific bacterial imbalances, digestive function markers, and inflammatory indicators. It’s crucial to avoid self-treating based solely on the report; incorrect supplementation or dietary changes could potentially worsen symptoms. Always work with a qualified professional.
Beyond Bacteria: The Importance of Functional Testing
Traditional stool tests often focus primarily on identifying pathogens. Gut panels go much further by assessing functional aspects of digestion and microbial activity. This means looking beyond simply who is present in your gut to understand what they’re doing. For example, a test might evaluate levels of zonulin – a protein that regulates intestinal permeability (often referred to as “leaky gut”).
- Elevated zonulin suggests increased intestinal permeability, which can allow undigested food particles and toxins to enter the bloodstream, potentially triggering immune responses.
- SCFA analysis provides insight into how well beneficial bacteria are fermenting fiber and producing these important metabolites. Low levels of SCFAs could indicate a lack of dietary fiber or an imbalance in gut flora.
- Digestive enzyme markers like elastase can reveal deficiencies in pancreatic function, which may hinder proper food breakdown and absorption.
This functional approach provides a more holistic understanding of gut health and allows for targeted interventions to restore optimal digestive function and microbial activity. This is particularly important because symptoms often arise from how the gut is functioning, not just which microbes are present. A colon imaging study might be helpful in some cases, understanding which symptoms can help guide this decision.
Integrating Gut Panel Results into a Holistic Plan
A gut panel isn’t a quick fix; it’s a starting point for a long-term health strategy. Once results are interpreted, your healthcare provider will work with you to develop a personalized plan that may include:
- Dietary Modifications: This could involve eliminating trigger foods identified through the test or incorporating more fiber-rich foods to nourish beneficial bacteria. Consider meal simplification techniques for ease of implementation.
- Probiotic and Prebiotic Supplementation: Selecting specific strains of probiotics based on your individual needs and pairing them with prebiotics (foods that feed beneficial bacteria).
- Lifestyle Changes: Managing stress, prioritizing sleep, and engaging in regular physical activity are all crucial for gut health.
- Addressing Underlying Issues: Identifying and addressing factors like food sensitivities, chronic inflammation, or hormonal imbalances that may be contributing to gut dysfunction.
It’s important to remember that restoring gut health is a process. It requires consistency, patience, and ongoing monitoring. Follow-up testing might be recommended to assess progress and make adjustments to the plan as needed. The ultimate goal is not just symptom relief but long-term wellbeing. By understanding your gut microbiome and addressing any imbalances, you can lay the foundation for a healthier, more resilient future. An MRI might offer additional insight in certain circumstances.