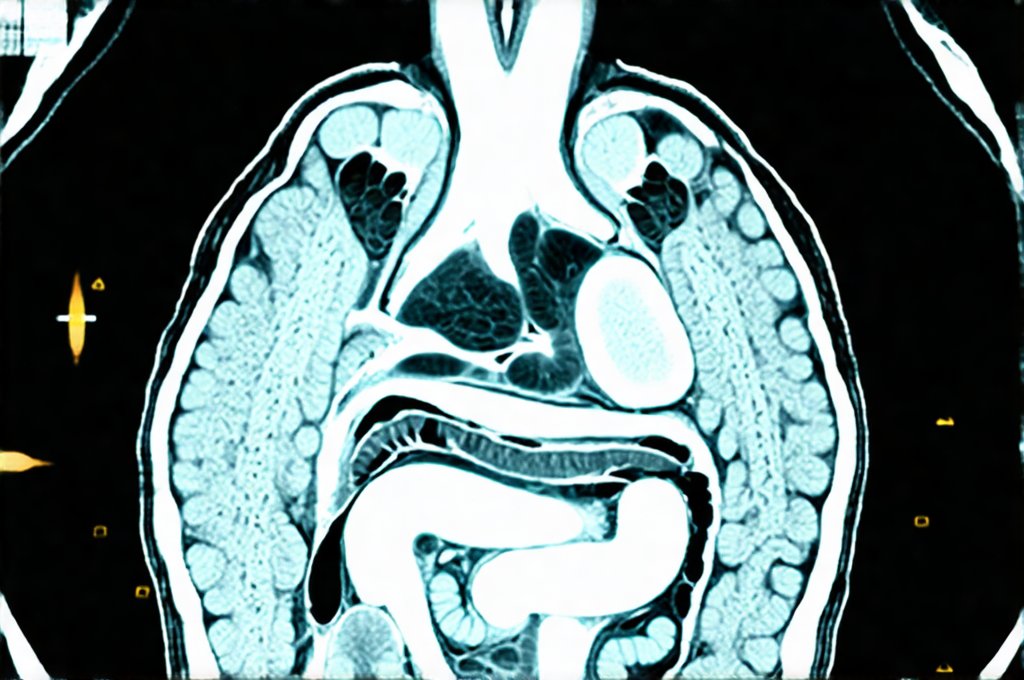
Gastrointestinal (GI) issues are remarkably common, affecting millions worldwide. From subtle discomfort to debilitating pain, these problems can significantly impact quality of life. Diagnosing the root cause often requires sophisticated imaging techniques, with both Computed Tomography (CT) scans and Magnetic Resonance Imaging (MRI) frequently employed. While CT has historically been the go-to for many GI investigations due to its speed and accessibility, MRI is increasingly recognized as a superior option in specific scenarios – offering detailed insights without some of the drawbacks associated with CT radiation and contrast agents. Understanding when an MRI surpasses a CT scan requires delving into the strengths and limitations of each modality, focusing on how they visualize different aspects of the gut and surrounding structures.
The choice between these two imaging methods isn’t always straightforward; it depends heavily on the specific clinical presentation, suspected diagnosis, and individual patient factors. A crucial consideration is that while CT excels at quickly identifying structural abnormalities like bowel obstructions or perforations, MRI often provides a more nuanced assessment of soft tissue inflammation, subtle disease processes, and functional issues within the GI tract. This article will explore these differences in detail, clarifying when an MRI becomes the preferred imaging choice for evaluating gut-related health concerns. It’s important to remember that this information is for educational purposes only and should not be interpreted as medical advice; always consult with a qualified healthcare professional for personalized guidance. Considering factors like diet and lifestyle can also support gut health – explore meal simplification techniques for a happy gut.
The Strengths of MRI in Gut Imaging
MRI offers several distinct advantages when it comes to investigating GI issues, particularly concerning the small bowel and surrounding areas. Unlike CT scans, which use ionizing radiation, MRI utilizes strong magnetic fields and radio waves, eliminating exposure to harmful radiation – a significant benefit especially for patients requiring repeated imaging or those with heightened sensitivity to radiation (like children). This makes MRI a safer option in the long term. Furthermore, MRI provides superior soft tissue contrast, allowing for clearer visualization of inflammation, tumors, fistulas, and other subtle abnormalities that might be missed on CT. This enhanced detail is critical when evaluating conditions like Crohn’s disease or ulcerative colitis where early detection and precise assessment are vital for effective management.
The ability to perform MR enterography (MRE) and MR cholangiopancreatography (MRCP) further expands MRI’s diagnostic capabilities. MRE specifically focuses on the small bowel, utilizing oral contrast agents to visualize the intestinal lumen and wall in great detail. MRCP provides detailed imaging of the bile ducts and pancreatic duct, aiding in the diagnosis of conditions like gallstones, pancreatitis, or tumors. These dedicated protocols allow for a comprehensive evaluation that goes beyond what standard CT scans can offer. In essence, MRI doesn’t just show what is there; it reveals how things are functioning at a more granular level. Understanding your triggers is also important – is alcohol a common trigger for digestive issues ?
Finally, advanced techniques like diffusion-weighted imaging (DWI) – which assesses the movement of water molecules within tissues – allow for early detection of subtle changes indicative of inflammation or tumor growth. This is particularly useful in differentiating between benign and malignant lesions. The increased sensitivity of MRI means smaller abnormalities can be identified earlier, potentially leading to improved treatment outcomes.
Assessing Crohn’s Disease and Ulcerative Colitis
Crohn’s disease and ulcerative colitis (inflammatory bowel diseases – IBD) are chronic inflammatory conditions that require accurate diagnosis and ongoing monitoring. While CT enterography is sometimes used for initial assessment, MRI has become the gold standard for evaluating both conditions, especially in areas like detecting fistulas, abscesses, and assessing disease activity. This is because MRI excels at visualizing the subtle inflammation within the bowel wall, which is a hallmark of IBD.
- Fistula detection: MRI can identify even small fistulas – abnormal connections between the intestine and other organs or skin – with greater accuracy than CT. This is crucial for surgical planning.
- Disease activity assessment: MRI allows clinicians to assess the extent and severity of inflammation, helping guide treatment decisions and monitor response to therapy. Active inflammation appears brighter on certain MRI sequences, providing a clear visual indication of disease status.
- Complications detection: MRI can identify complications like strictures (narrowing of the intestine) or abscesses more reliably than CT.
The avoidance of radiation is also particularly important in IBD patients who often require frequent imaging for monitoring their condition over time. Repeated CT scans expose them to cumulative radiation dose, increasing the risk of long-term health effects. MRI provides a safe and effective alternative. The detailed information provided by MRI allows for more personalized treatment plans, ultimately improving patient outcomes. If you are experiencing ongoing gut distress, when rest is the only remedy for functional gut distress may offer some relief.
Evaluating Small Bowel Disease Beyond IBD
The small bowel presents unique imaging challenges due to its length and complex anatomy. CT enterography has traditionally been used to evaluate small bowel disease, but MRE – an MRI-based technique – offers significant advantages. MRE provides superior visualization of the small bowel wall, making it ideal for detecting subtle signs of inflammation, tumors, or other abnormalities. The use of oral contrast agents during MRE helps distend the bowel, improving image quality and facilitating accurate diagnosis.
Celiac disease, though often diagnosed through blood tests and endoscopy, can sometimes require imaging to assess complications like refractory celiac disease or lymphoma. MRI can help identify subtle changes in the small bowel wall associated with these conditions. Similarly, small intestinal bacterial overgrowth (SIBO), although typically diagnosed through breath testing, might necessitate imaging to rule out structural abnormalities contributing to the overgrowth. MRI can detect signs of chronic inflammation or malabsorption that may be present in SIBO patients.
Moreover, MRI is exceptionally useful for evaluating tumors within the small bowel. It provides detailed information about tumor size, location, and spread, aiding in surgical planning and treatment decisions. The ability to differentiate between benign and malignant lesions with high accuracy further enhances its diagnostic value. Is intermittent fasting helpful for gut issues is also a question many patients ask, as diet impacts health.
Differentiating Between Benign and Malignant Lesions
One of the most critical applications of MRI in gut imaging is its ability to distinguish between benign (non-cancerous) and malignant (cancerous) tumors. While CT can identify structural abnormalities, it often struggles to reliably differentiate between these two. MRI, with its superior soft tissue contrast and advanced techniques like DWI, offers a more accurate assessment.
DWI, as mentioned earlier, detects changes in water molecule movement within tissues. Cancer cells typically have restricted diffusion – meaning water molecules struggle to move freely within them – resulting in brighter signals on DWI images. This helps identify cancerous lesions with greater confidence. Furthermore, MRI can assess the extent of tumor spread and involvement of surrounding structures, providing crucial information for staging cancer and guiding treatment decisions.
- Tumor characterization: MRI provides detailed information about tumor characteristics, such as size, shape, margins, and internal structure.
- Lymph node evaluation: MRI can accurately assess lymph nodes for signs of metastasis (cancer spread).
- Vascular involvement: MRI can determine if the tumor is encroaching on or compressing blood vessels, which is important for surgical planning.
In conclusion, while CT remains a valuable tool in gut imaging, particularly for emergency situations requiring rapid assessment of acute problems like bowel obstruction, MRI has emerged as the preferred modality in numerous scenarios – especially those demanding detailed evaluation of soft tissues, subtle disease processes, and functional issues within the GI tract. The benefits of avoiding radiation exposure, superior soft tissue contrast, and advanced techniques like MRE and DWI make MRI a powerful diagnostic tool for patients with gut-related health concerns. Always consult your physician to determine which imaging modality is most appropriate for your specific situation. To support overall wellbeing alongside diagnostics, consider evening wind-down practices for a calm gut. Finally, exploring minimalist eating approaches for a calmer gut can also be beneficial.