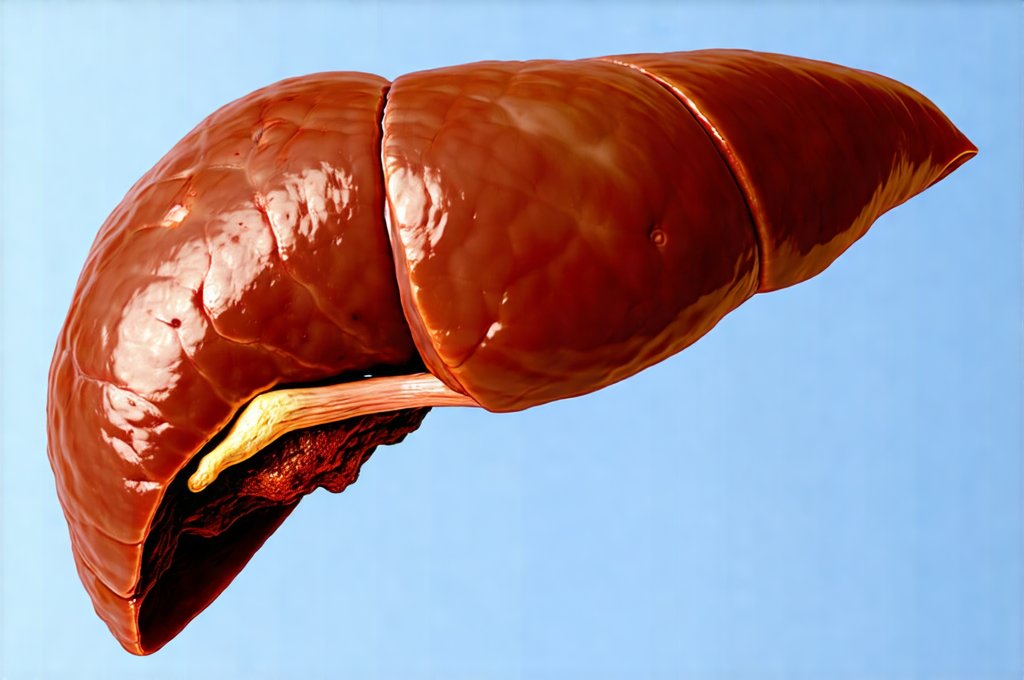
The liver is arguably one of the most versatile organs in the human body, performing over 500 essential functions – from filtering toxins and processing nutrients to producing vital proteins and bile for digestion. Assessing its health is therefore paramount, and clinicians rely on a range of diagnostic tools to do so. Blood tests are often the first line of investigation, providing valuable insights into liver enzyme levels, bilirubin concentrations, and protein synthesis capacity. However, blood tests paint a picture based on indirect evidence; they tell us about what the liver is doing, not necessarily what the liver looks like or how it’s physically structured. This is where liver scans come in – offering a direct visualization of the organ itself and providing information that blood tests simply cannot reveal.
While blood tests are excellent at detecting functional abnormalities, such as inflammation or damage, they can sometimes be normal even when structural problems exist within the liver. For example, early stages of fibrosis (scarring) might not significantly elevate enzyme levels, or a small tumor could be present without causing dramatic changes in blood work. Similarly, conditions affecting bile ducts – crucial for draining waste from the liver – may initially show subtle signs on blood tests before becoming clinically apparent. Liver scans offer a complementary approach, allowing clinicians to identify these structural issues early and more accurately, leading to better patient management and outcomes. They are not meant to replace blood tests but rather to enhance diagnostic precision when needed.
Understanding the Limitations of Blood Tests & The Role of Imaging
Blood tests related to liver health primarily measure markers of damage or dysfunction. Elevated alanine aminotransferase (ALT) and aspartate aminotransferase (AST) indicate liver cell injury, while elevated bilirubin suggests impaired bile excretion. However, these elevations are often non-specific – meaning they can be caused by a variety of conditions, ranging from mild inflammation to severe cirrhosis. A blood test might tell you that something is wrong, but not what or where. Furthermore, blood tests reflect the average state of the liver over a period of time; they don’t provide information about localized abnormalities like tumors or abscesses that may be present within the organ.
Liver scans, on the other hand, offer a spatial understanding of the liver. They create images that allow doctors to see the size and shape of the liver, identify any masses or lesions, assess blood flow within the organ, and evaluate the condition of the bile ducts. Different types of scans provide varying levels of detail and are chosen based on the clinical question being asked. This direct visualization is invaluable for differentiating between various conditions and guiding treatment decisions. For instance, distinguishing between benign growths and malignant tumors often requires imaging beyond what blood tests can offer.
Consider a patient presenting with mildly elevated liver enzymes. A blood test might suggest hepatitis or early fatty liver disease. However, if the physician suspects a more serious underlying condition like a tumor or abscess, a liver scan becomes crucial for definitive diagnosis. It’s about building a complete picture – integrating information from both blood tests and imaging studies to arrive at an accurate assessment of liver health. The synergy between these diagnostic tools is what ensures optimal patient care. If you are concerned about your gas, it could be a sign of something more serious — serious condition.
When Liver Scans Become Essential: Specific Scenarios
A liver scan isn’t routinely performed for every patient with suspected liver issues; it’s reserved for situations where blood tests are inconclusive, raise specific concerns, or require further investigation. Here are some key scenarios where a liver scan is demonstrably more useful than relying solely on blood work:
- Suspected Liver Tumors: Blood tests may not detect small tumors early on. Scans like CT or MRI can identify even tiny lesions, determine their location and size, and help differentiate between benign and malignant growths. This early detection dramatically improves treatment outcomes.
- Evaluation of Bile Duct Obstruction: If a patient presents with jaundice (yellowing of the skin and eyes) or elevated bilirubin levels, a scan is often necessary to identify any blockage in the bile ducts, which could be caused by gallstones, tumors, or strictures. Ultrasound, CT, or MRI can visualize the biliary system and pinpoint the site of obstruction.
- Assessment of Liver Cirrhosis Severity: While blood tests can indicate the presence of cirrhosis, scans (particularly MRI) can assess its stage and extent. This helps doctors determine the prognosis and guide treatment decisions, such as whether a liver transplant is necessary.
Types of Liver Scans & Their Strengths
There are several different types of liver scans available, each with its own advantages and disadvantages. The choice of scan depends on the specific clinical question being asked and the patient’s individual circumstances:
- Ultrasound: This non-invasive technique uses sound waves to create images of the liver. It’s relatively inexpensive, readily available, and doesn’t involve radiation. Ultrasound is excellent for detecting gallstones, assessing bile duct dilation, and identifying large masses. However, it can be limited by patient body habitus (size) and may not visualize small lesions as clearly as other methods.
- Computed Tomography (CT Scan): CT scans use X-rays to create cross-sectional images of the liver. They provide detailed anatomical information and are particularly good at detecting tumors, abscesses, and vascular abnormalities. However, CT scans involve radiation exposure, which is a concern for some patients.
- Magnetic Resonance Imaging (MRI): MRI uses magnetic fields and radio waves to create highly detailed images of the liver. It offers superior soft tissue contrast compared to CT scans, making it ideal for detecting small lesions, assessing fibrosis, and evaluating bile ducts. MRI doesn’t involve radiation but is more expensive and time-consuming than CT scans. A specific type of MRI called MRCP (Magnetic Resonance Cholangiopancreatography) is particularly useful for visualizing the biliary system. You may also want to understand acid reflux and if it’s a more serious condition.
Further Considerations & Future Trends
It’s important to remember that liver scans are not without their limitations. They can sometimes produce false positives or false negatives, and interpretation requires expertise. Clinicians must carefully correlate scan findings with blood test results and clinical history to arrive at an accurate diagnosis. Furthermore, the use of contrast agents in CT and MRI carries a small risk of allergic reactions or kidney problems, so patient suitability must be assessed beforehand. If you’re experiencing digestive issues, leaky gut syndrome could be a factor.
Looking ahead, advancements in imaging technology are continuously improving the accuracy and efficiency of liver scans. Techniques like elastography (assessing liver stiffness) and functional MRI (measuring blood flow and metabolic activity) are becoming increasingly sophisticated and provide even more detailed information about liver health. Artificial intelligence is also being integrated into image analysis, helping radiologists detect subtle abnormalities and improve diagnostic accuracy. These developments promise to further enhance our ability to diagnose and manage liver diseases effectively. The future of liver health assessment lies in a combined approach – leveraging the strengths of both blood tests and advanced imaging techniques for personalized and precise patient care. If you are concerned about high blood pressure, GERD may be related. Remember to always practice food safety. A healthy diet can also help, particularly when breaking a fast.