A routine physical exam often feels like a checklist – weight, blood pressure, maybe a quick listen to your heart. But tucked within that broader assessment is a significant focus on your gut health, even if it doesn’t always feel explicitly addressed. This isn’t merely about identifying obvious problems; it’s about gathering crucial information about your overall well-being, as the gastrointestinal system profoundly impacts everything from nutrient absorption and immune function to mental health. Understanding what to ask your doctor before a gut exam can empower you to be an active participant in your healthcare and potentially identify issues early on.
The gut isn’t just a passive digestive tract; it’s a complex ecosystem, home to trillions of microorganisms – the gut microbiome – that play vital roles in health. A doctor’s assessment during a physical incorporates both what you report (your symptoms) and what they observe through examination and potentially further testing. It’s a holistic approach designed to paint a comprehensive picture of your digestive function and identify any areas requiring closer attention. This often involves questions about bowel habits, diet, and family history alongside a physical palpation of the abdomen, and sometimes, depending on presenting concerns or age, more detailed investigations. Recognizing gut microbiome signs is important for overall health.
What Does the Doctor Ask About?
The initial part of a gut assessment usually begins with a thorough conversation. Doctors are skilled at using open-ended questions to get a clear understanding of your digestive health. Expect questions about: – Frequency and consistency of bowel movements – Are you regular? Have there been changes? – Presence of any pain, bloating, gas, or cramping. Where is the pain located? What makes it better or worse? – Changes in appetite or unintentional weight loss/gain. – Any blood in your stool, or changes in stool color. – Family history of gastrointestinal conditions like Crohn’s disease, ulcerative colitis, colon cancer, or celiac disease. – Your diet – what do you typically eat and drink? Do you have any food intolerances or allergies? – Medications you are currently taking, including over-the-counter drugs and supplements.
This detailed questioning isn’t just about identifying current problems; it’s also about establishing a baseline for future comparisons. Chronic symptoms or subtle changes often come to light during these conversations, which might otherwise go unnoticed. Your doctor is looking for patterns and red flags that signal the need for further investigation. Open and honest communication is key here – don’t hesitate to share even seemingly minor details. It’s also important to remember that there’s no such thing as a “stupid question” when it comes to your health. When you are overeating, consider how to reset your gut afterwards.
The doctor isn’t just interested in the what of your symptoms, but also the how and when. For example, noting if bloating worsens after certain foods or if pain is triggered by stress can provide valuable clues about underlying causes. Furthermore, they’ll want to know how these symptoms impact your daily life – are they interfering with work, social activities, or sleep? This helps them gauge the severity of the issue and determine appropriate next steps. If you’re busy, knowing what to eat can help avoid digestive issues.
The Physical Examination: Palpation and Auscultation
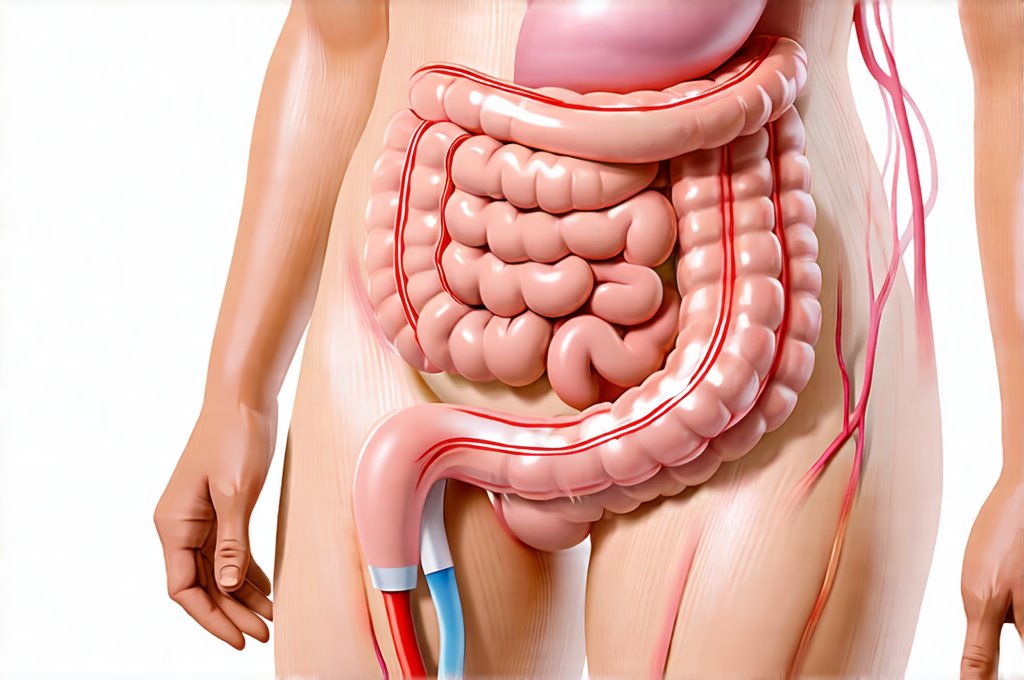
After gathering information through questioning, the doctor will move on to a physical examination focusing on your abdomen. Palpation – gently pressing on different areas of your abdomen – is a key component. This isn’t meant to cause pain; it’s about assessing for tenderness, masses, or distention (swelling). The doctor systematically examines each quadrant of your abdomen: upper right, upper left, lower right, and lower left. They are feeling for signs of inflammation, organ enlargement, or areas of discomfort.
The doctor is also listening – using a stethoscope to perform auscultation. This involves listening to the sounds within your abdomen. Normal bowel sounds are gurgling and irregular. Absent or excessively loud sounds can indicate problems with intestinal motility (movement). For example, high-pitched tinkling sounds might suggest an obstruction, while quiet or absent sounds could point to ileus (temporary loss of intestinal function). Auscultation helps the doctor assess how well your digestive system is functioning mechanically.
The physical exam isn’t solely focused on what the doctor finds abnormal. They are also assessing for general muscle tone and any signs of guarding – tensing of abdominal muscles in response to discomfort. The way you react during palpation provides additional information about your pain tolerance and potential areas of concern. A gentle, methodical approach is crucial to ensure a comfortable experience and accurate assessment.
Further Investigations: When are Tests Needed?
Based on the initial assessment – both questioning and physical exam – your doctor may recommend further investigations. These aren’t always necessary, but they can provide more definitive answers if there’s suspicion of an underlying condition. Common tests include: – Stool tests: to check for infections (bacteria, parasites), blood, or inflammation. – Blood tests: to assess organ function, look for signs of anemia, and screen for celiac disease or inflammatory bowel disease markers. – Colonoscopy/Endoscopy: These involve using a flexible camera to visualize the inside of the colon or esophagus/stomach, respectively. They are often used to investigate symptoms like rectal bleeding, chronic diarrhea, or unexplained weight loss. – Imaging studies (CT scan, MRI): Can help identify structural abnormalities in the digestive tract.
The choice of tests depends entirely on your individual symptoms and medical history. Your doctor will explain the rationale behind each test and what to expect during the process. It’s important to ask questions if you have any concerns or uncertainties about these investigations. Testing isn’t a sign of something being seriously wrong – it’s simply a way to gather more information and make an accurate diagnosis. If you experience reflux flare-ups, understanding how to soothe your system is helpful. Understanding belching frequency can also provide insight into gut function.
The goal of all these assessments – questioning, physical exam, and potential testing – is not just to identify problems but also to promote preventative care. By understanding your gut health and addressing any concerns early on, you can take proactive steps to maintain optimal digestive function and overall well-being. Remember that a healthy gut is fundamental to a healthy life, and partnering with your doctor is the best way to ensure it stays that way.