The gut microbiome – the vast ecosystem of bacteria, fungi, viruses, and other microorganisms residing in our digestive tract – is increasingly recognized as central to overall health. Beyond simply digesting food, this complex community profoundly impacts immunity, mental wellbeing, hormone regulation, and even chronic disease risk. When imbalances occur within this intricate system, symptoms can range from bloating and gas to fatigue, skin problems, and autoimmune flares. Identifying these imbalances isn’t always straightforward, which is where comprehensive stool analysis comes into play. This testing method offers a detailed snapshot of the gut microbiome, providing insights that traditional diagnostic methods often miss.
Comprehensive stool analysis differs significantly from routine stool tests typically ordered by physicians for infection detection. While basic stool tests look for things like blood or parasites, a comprehensive analysis delves much deeper, examining microbial composition, digestive function, inflammation markers, and nutrient absorption. It’s not simply about identifying “bad” bacteria; it’s about understanding the entire ecosystem – the balance between beneficial and potentially problematic organisms, how well your body is digesting food, and whether there are signs of gut irritation or immune activation. This information can then be used to tailor dietary interventions, lifestyle changes, and targeted supplementation strategies aimed at restoring a healthier gut environment.
Understanding What’s Measured in a Comprehensive Stool Analysis
A comprehensive stool analysis isn’t a single test; it’s typically a panel of many different measurements. These tests aim to paint a detailed picture of the gut ecosystem, moving beyond just identifying what organisms are present. They examine the quantity and diversity of microbial life, looking at both bacteria and other microorganisms like fungi and parasites. Different labs use varying methodologies – some utilizing DNA sequencing (like 16S rRNA gene sequencing) for bacterial identification while others employ culture-based techniques or immunological assays to detect specific markers. The goal is always to create a holistic understanding of the gut’s functionality.
Crucially, these analyses don’t merely list organisms; they often provide comparative data against established “normal” ranges. This allows practitioners to assess whether levels are deficient, excessive, or out of balance. Beyond microbial composition, tests evaluate markers related to digestive sufficiency. These include measurements of pancreatic elastase (indicating pancreatic function), fecal fat content (assessing fat absorption), and levels of lysozyme (an antibacterial enzyme). Detecting deficiencies in these areas can indicate malabsorption issues or inadequate digestive capacity.
Finally, comprehensive stool analyses often incorporate inflammatory markers like calprotectin and lactoferrin, which signal the presence of gut inflammation. Elevated levels may suggest conditions like Inflammatory Bowel Disease (IBD) or increased intestinal permeability (“leaky gut”). These tests are invaluable for identifying potential imbalances and guiding targeted interventions to support a healthier digestive system. It’s important to remember that results should always be interpreted by a qualified healthcare professional, as the microbiome is incredibly complex and requires nuanced understanding. If you suspect an issue, it’s best to understand what you need to know before testing.
The Process of Stool Collection & Interpretation
The process of collecting a stool sample for analysis is relatively straightforward, but adherence to specific instructions is vital for accurate results. Most labs provide detailed collection kits with clear guidelines. Generally, this involves: – Using a special collection container provided by the lab – Avoiding certain medications or dietary changes prior to testing (as specified by the lab) – Collecting a small amount of stool directly into the container – often avoiding toilet water contamination – Promptly freezing and shipping the sample to the laboratory according to their instructions.
The turnaround time for results varies depending on the lab, but typically ranges from one to three weeks. Once received, the data is analyzed and presented in a comprehensive report. This report will outline findings related to microbial diversity, specific bacterial populations, digestive markers, inflammation indicators, and other relevant parameters. However, the raw data itself isn’t particularly useful without proper interpretation.
This is where a healthcare practitioner specializing in gut health becomes invaluable. They can translate complex results into actionable insights. Interpretation involves not only the numerical values but also the patient’s individual symptoms, medical history, and lifestyle factors. It’s critical to avoid self-diagnosing based on stool analysis results. A skilled clinician will identify patterns, prioritize areas of concern, and develop a personalized plan to address any imbalances. This might include dietary modifications, prebiotic or probiotic supplementation, stress management techniques, or other supportive therapies. Understanding gut motility can also aid in this process.
Understanding Key Microbial Markers
Within the comprehensive stool analysis report, several microbial markers are particularly important for understanding gut health. Bacterial diversity is often one of the first things clinicians look at. A higher degree of diversity generally indicates a more resilient and stable ecosystem. Low diversity can be associated with increased susceptibility to illness and chronic disease. Specific bacterial groups also provide valuable information. For example: – Increased levels of Firmicutes relative to Bacteroidetes have been linked to obesity in some studies, though the relationship is complex. – The presence of certain opportunistic pathogens like Klebsiella or Clostridium difficile may indicate dysbiosis and require targeted intervention. – Beneficial bacteria such as Lactobacillus and Bifidobacterium are often associated with improved gut health and immune function, and low levels can suggest a need for probiotic support.
It’s crucial to remember that these bacterial populations aren’t isolated entities; they interact with each other in complex ways. A healthy microbiome isn’t just about having more “good” bacteria—it’s about achieving a balanced ecosystem where different species coexist harmoniously. Furthermore, the relative abundance of these organisms is often more important than their absolute numbers. Looking at ratios and relationships between different groups can provide deeper insights into gut function.
Interpreting Digestive Sufficiency Markers
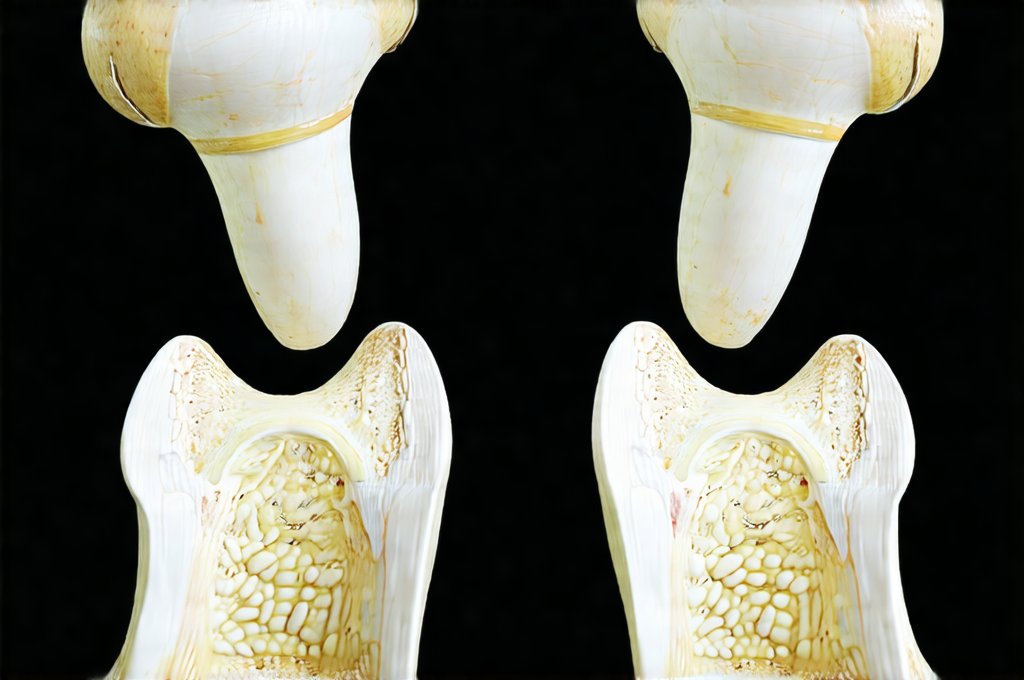
Beyond microbial composition, comprehensive stool analysis provides valuable information about digestive capacity. Pancreatic elastase-1 (PE1) is a key marker for pancreatic function. Low levels indicate insufficient pancreatic enzyme production, potentially leading to malabsorption of fats and proteins. Fecal fat content measures the amount of undigested fat in the stool. Elevated levels suggest impaired fat absorption, which can result from inadequate bile acid production, pancreatic insufficiency, or small intestinal dysfunction.
Lysozyme is an antibacterial enzyme found in the intestines, offering some level of immune defense. While a certain amount is normal and healthy, very low levels might indicate reduced gut barrier function or compromised immunity. Other digestive markers may include measurements of short-chain fatty acids (SCFAs), which are produced by bacterial fermentation of dietary fiber and play crucial roles in gut health and overall wellbeing. Low SCFA production can indicate insufficient fiber intake or imbalances in the microbiome. Analyzing these digestive sufficiency markers helps identify areas where digestive processes might be compromised, allowing for targeted interventions to improve nutrient absorption and reduce gastrointestinal symptoms.
Addressing Inflammation & Gut Permeability
Inflammation is a common feature of many gut-related conditions, and comprehensive stool analysis can help assess its presence. Calprotectin and lactoferrin are two key markers used to detect inflammation in the intestines. Elevated levels typically indicate active inflammation, potentially suggesting IBD, food sensitivities, or other underlying issues. It’s important to note that these markers aren’t specific to any particular condition but rather signal the presence of immune activation within the gut.
Gut permeability, often referred to as “leaky gut,” is another area assessed in some comprehensive stool analyses. While direct measurement of intestinal permeability isn’t always possible through stool testing, certain markers can provide indirect clues. For example, elevated levels of zonulin—a protein that regulates intestinal barrier function – may suggest increased permeability. A compromised gut barrier allows undigested food particles and toxins to enter the bloodstream, potentially triggering immune responses and contributing to systemic inflammation. Addressing gut permeability often involves dietary changes (such as eliminating inflammatory foods), supporting gut healing with nutrients like glutamine and zinc, and restoring a balanced microbiome to strengthen the intestinal barrier. Remember that these markers provide valuable clues but require careful interpretation within the context of the patient’s overall health picture. If you’re experiencing reflux symptoms, consider what to include in a reflux-rescue kit. You may also want to learn about a low histamine diet if food sensitivities are suspected. Finally, understanding what happens after a flare up can help manage ongoing symptoms.