Heartburn is one of those incredibly common experiences – something many of us have dealt with at least once, if not regularly. It’s often associated with indulging in rich, spicy, or fatty foods, but what about when it strikes even when your stomach is empty? This seemingly paradoxical situation can be particularly frustrating and concerning, leading people to wonder what exactly is going on within their bodies. The discomfort isn’t just a simple case of too much food; it’s frequently indicative of more complex interactions between our digestive system, lifestyle factors, and even psychological state. Understanding these underlying mechanisms is crucial for effectively managing heartburn and minimizing its impact on daily life.
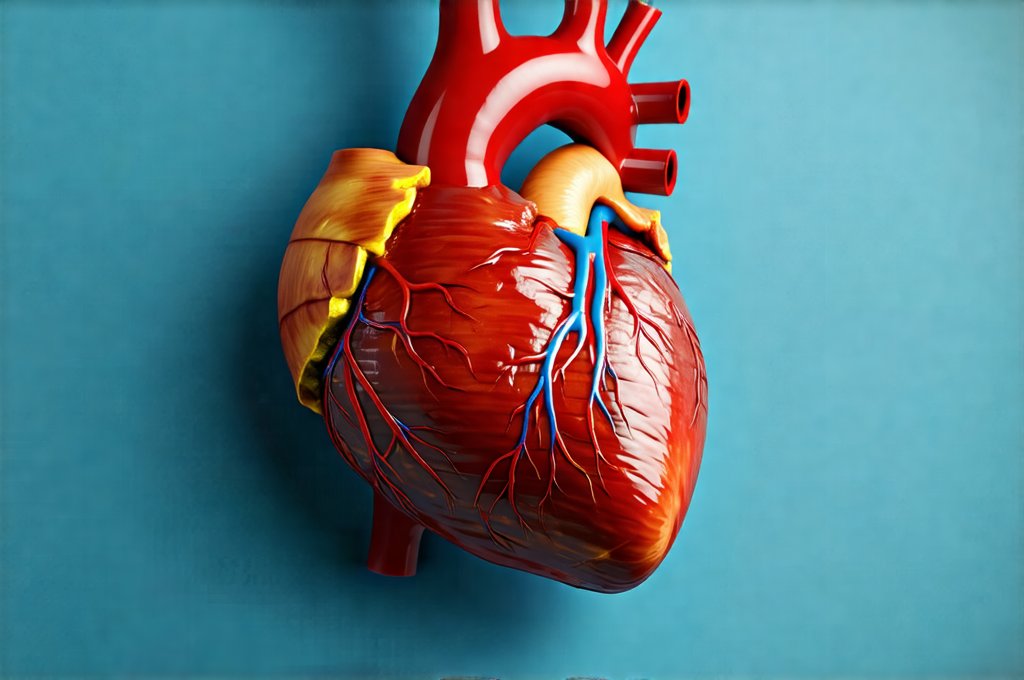
The sensation we call “heartburn” isn’t actually related to the heart at all. It’s a burning feeling in the chest that arises from stomach acid flowing back up into the esophagus – the tube connecting your mouth to your stomach. This backward flow, known as acid reflux, irritates the sensitive lining of the esophagus, triggering the familiar discomfort. While overeating certainly exacerbates this process, it doesn’t fully explain why heartburn can occur even when you haven’t eaten recently or have only consumed a small amount of food. The body is a complex system and numerous factors beyond dietary intake contribute to acid reflux episodes. This article delves into those factors, offering a comprehensive look at what really triggers heartburn, particularly on an empty stomach.
The Lower Esophageal Sphincter: A Key Player
The lower esophageal sphincter (LES) is the muscular ring at the bottom of your esophagus that acts as a valve between the esophagus and the stomach. Its primary function is to prevent stomach acid from flowing back up. When you swallow, the LES relaxes to allow food and liquids to pass into the stomach, then tightens afterwards to seal things off. A weakened or malfunctioning LES is often at the heart of heartburn, even when your stomach appears empty. Several factors can compromise its function:
- Certain foods like peppermint, chocolate, and caffeine can temporarily relax the LES.
- Habitual overeating stretches the LES over time, diminishing its ability to close properly.
- Lifestyle choices such as smoking and excessive alcohol consumption also weaken this crucial muscle.
- Hiatal hernia, a condition where part of the stomach protrudes through the diaphragm, can physically disrupt the LES’s function.
Even without recent food intake, acid is still present in the stomach – it’s necessary for digestion. If the LES isn’t functioning effectively, even small amounts of this existing acid can reflux into the esophagus, causing heartburn. This explains why you might experience symptoms hours after your last meal or even overnight while sleeping. The position of your body also plays a role; lying down makes it easier for stomach acid to flow upwards.
The LES isn’t always “on” or “off.” It’s constantly undergoing transient relaxations – moments when it briefly opens, even without swallowing. These are called transient lower esophageal sphincter relaxations (TLESRs) and they are a natural part of the digestive process. However, if TLESRs occur too frequently or last too long, acid reflux is more likely to happen. Individuals prone to heartburn often experience more frequent and prolonged TLESRs than others. Understanding what bloating says about your digestive system can help you better understand these reactions.
Stress and Heartburn: A Surprising Connection
While we often associate heartburn with food, the link between stress and this uncomfortable sensation is significant. When you’re stressed, your body activates the “fight-or-flight” response, releasing hormones like cortisol. This can have several effects that contribute to acid reflux and heartburn:
- Increased stomach acid production: Cortisol stimulates the production of gastric acid, potentially overwhelming the LES’s ability to contain it.
- Weakened LES function: Stress can directly cause the LES to relax more frequently, making reflux more likely.
- Disrupted digestive processes: Stress slows down digestion, leaving food in your stomach longer and increasing the risk of acid buildup.
It’s important to note that stress isn’t just about major life events; even chronic, low-level stress can contribute to heartburn symptoms. Practices like meditation, deep breathing exercises, yoga, or simply taking time for relaxation can all help manage stress levels and potentially reduce the frequency of heartburn episodes. Mindful awareness of your stress triggers is a crucial step toward managing this connection. If you’re struggling with what to cook when everything seems to cause issues, remember that stress can exacerbate the problem.
The Role of Body Position & Timing
The way you position your body, especially after “eating” (even if it’s just drinking water), significantly impacts acid reflux. Gravity plays a role – when you lie down or bend over, it’s easier for stomach acid to travel upwards into the esophagus. This is why heartburn often worsens at night.
- Elevating the head of your bed by 6-8 inches can help keep acid in the stomach while you sleep.
- Avoiding lying down immediately after consuming anything, even liquids, gives your LES time to close and reduces the likelihood of reflux.
- Maintaining good posture throughout the day helps prevent pressure on the abdomen, which can contribute to acid reflux.
The timing of symptoms is also important. Heartburn that occurs shortly after “eating” (even a small snack) might indicate a dietary trigger or LES malfunction. However, heartburn that develops several hours later could be linked to nighttime acid production or TLESRs. Identifying the pattern and timing can help pinpoint the underlying cause and guide appropriate management strategies. Consider what to avoid on an anti-inflammatory diet if you suspect food sensitivities are at play.
Medications & Underlying Conditions
Certain medications can exacerbate heartburn symptoms by relaxing the LES or increasing stomach acid production. Some common culprits include:
- Calcium channel blockers for high blood pressure
- Anticholinergics for overactive bladder
- Some pain relievers and anti-inflammatory drugs
- Certain antidepressants
If you suspect a medication is contributing to your heartburn, always consult with your doctor before stopping or changing any prescribed medications. Never self-medicate.
Beyond lifestyle factors and medication side effects, underlying medical conditions can also play a role in chronic heartburn. Gastroesophageal Reflux Disease (GERD) is a more serious form of acid reflux where the condition is frequent and causes significant symptoms or complications. Other potential contributing conditions include:
- Peptic ulcers: Sores in the lining of the stomach or duodenum can increase acid production.
- Gastroparesis: Delayed stomach emptying can lead to increased pressure and reflux.
- Scleroderma: A rare autoimmune disease that affects the digestive system, potentially weakening the LES.
It is vital to seek medical attention if heartburn persists despite lifestyle modifications or is accompanied by other symptoms like difficulty swallowing, chest pain, vomiting, or unexplained weight loss. These could indicate a more serious underlying problem requiring diagnosis and treatment. To better understand your body’s signals, consider are there hidden triggers in your kitchen? A systematic approach can help you identify potential problems. And remember to track how to know if you’re really improving. Finally, it is important to be mindful of foods to be cautious with on an elimination diet if you suspect food sensitivities are contributing to your issues.