Chronic heartburn, an all-too-familiar discomfort for millions, is far more than just a temporary annoyance. It’s often a symptom signaling deeper changes occurring within the esophagus – the muscular tube responsible for transporting food from your mouth to your stomach. While occasional heartburn is common and usually easily managed, persistent symptoms indicate something isn’t functioning as it should, and prolonged exposure to stomach acid can inflict significant damage over time. Understanding what happens to your esophagus during chronic heartburn is crucial not only for recognizing potential health risks but also for proactively managing the condition and preventing long-term complications. It’s about more than just suppressing the burn; it’s about understanding why it’s happening in the first place and taking steps towards lasting esophageal health. If you are unsure what happens when you eat certain foods, consider looking into foods youre sensitive to.
The sensation of heartburn itself isn’t actually felt in the heart, despite its name. Instead, it’s a burning pain that rises from the chest – often mistaken for cardiac issues – caused by stomach acid refluxing back up into the esophagus. This happens when the lower esophageal sphincter (LES), a ring of muscle at the bottom of the esophagus, doesn’t close properly after food passes through. Several factors can contribute to this weakened closure, ranging from dietary choices and lifestyle habits to anatomical variations and underlying medical conditions. Ignoring chronic heartburn isn’t simply tolerating discomfort; it allows for progressive damage that can drastically alter esophageal function and potentially lead to serious health problems if left unaddressed. If your gut is inflamed, understanding what to eat may help ease symptoms.
The Escalation of Esophageal Damage
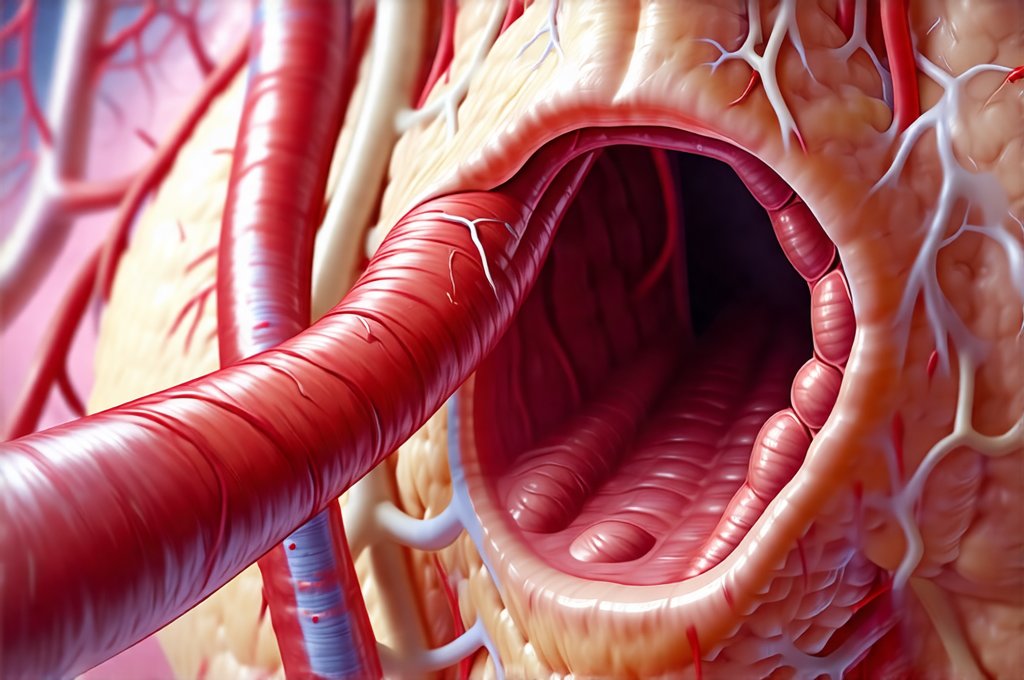
The esophagus is surprisingly resilient, but its protective mechanisms are limited when repeatedly exposed to acidic stomach contents. Normally, the esophageal lining has a natural defense system involving bicarbonate production – a mild alkaline substance that neutralizes some acid. However, chronic reflux overwhelms this system, leading to inflammation and gradual structural changes. Initially, this manifests as reflux esophagitis, where the lining becomes inflamed and irritated. This can cause symptoms beyond just heartburn, including difficulty swallowing (dysphagia), a sour taste in the mouth, and even chest pain that mimics heart attack symptoms. The severity of esophagitis depends on the frequency and amount of acid exposure, as well as individual susceptibility.
Over time, persistent inflammation triggers cellular changes within the esophageal lining. The body attempts to repair the damage, but instead of restoring normal tissue, it often leads to metaplasia. This is a process where cells change type – in this case, healthy squamous cells (the normal lining of the esophagus) are replaced with columnar cells that resemble those found in the intestine. This isn’t necessarily harmful initially, but it represents a significant alteration in esophageal structure and sets the stage for more serious complications down the line. Think of it as the body attempting to adapt, but using materials that aren’t ideal for the task at hand. It can be difficult to build trust with your body during times like these, so remember to take care of yourself.
The final, most concerning outcome of long-term, untreated chronic heartburn is Barrett’s esophagus. This occurs when a substantial portion of the esophageal lining has been replaced with intestinal-type cells. Barrett’s esophagus isn’t directly painful, and many individuals don’t even know they have it until complications arise. However, it significantly increases the risk of developing adenocarcinoma, a type of esophageal cancer. While only a small percentage of people with Barrett’s esophagus develop cancer, regular monitoring is essential for early detection and intervention. If you are unsure what to ask your doctor before a procedure, don’t hesitate to reach out!
Understanding Dysplasia & Cancer Risk
Dysplasia refers to abnormal cell growth that can occur within the context of Barrett’s esophagus. It’s considered a precancerous condition, meaning it increases the likelihood of developing esophageal cancer. There are two main grades of dysplasia: low-grade and high-grade. – Low-grade dysplasia indicates mild abnormalities, and while it doesn’t significantly increase immediate cancer risk, it requires ongoing monitoring to watch for progression. – High-grade dysplasia signifies more substantial cell changes and is considered a direct precursor to adenocarcinoma. Patients with high-grade dysplasia often require aggressive treatment options such as endoscopic ablation (removing the abnormal tissue) or even esophageal resection (surgical removal of part of the esophagus). Chronic gastritis can also be a factor, so understanding chronic gastritis is important too.
Regular surveillance, typically involving endoscopy with biopsies, is crucial for individuals diagnosed with Barrett’s esophagus. Endoscopy allows doctors to visualize the esophageal lining and collect tissue samples for microscopic examination, enabling them to detect dysplasia early on. The frequency of endoscopic monitoring depends on the presence and grade of dysplasia, as well as individual risk factors. Early detection of dysplasia significantly improves treatment outcomes and reduces the risk of developing esophageal cancer. It’s a proactive approach to managing a potentially serious condition.
Lifestyle & Dietary Modifications
While medical interventions are often necessary for managing chronic heartburn and its complications, lifestyle and dietary changes play a vital role in mitigating symptoms and slowing disease progression. These modifications aren’t about eliminating all enjoyable foods; they’re about making informed choices that minimize acid reflux and esophageal irritation. – Dietary adjustments: Avoiding trigger foods such as chocolate, caffeine, alcohol, fatty foods, spicy foods, and citrus fruits can significantly reduce heartburn frequency. Eating smaller, more frequent meals instead of large ones also helps to lessen pressure on the LES. – Lifestyle changes: Elevating the head of your bed by 6-8 inches during sleep can help prevent nighttime reflux. Avoiding lying down immediately after eating and maintaining a healthy weight are also beneficial strategies. – Smoking cessation: Smoking weakens the LES, increasing the risk of acid reflux. Quitting smoking is one of the most impactful steps you can take to improve esophageal health.
Medications & Interventions
For many individuals, medications offer effective relief from heartburn symptoms and help manage underlying conditions like GERD (gastroesophageal reflux disease). – Antacids: Provide quick but temporary relief by neutralizing stomach acid. They’re best for occasional heartburn rather than chronic management. – H2 Blockers: Reduce acid production in the stomach, offering longer-lasting relief than antacids. – Proton Pump Inhibitors (PPIs): The most potent class of acid-reducing medications. PPIs are often prescribed for severe GERD or Barrett’s esophagus to suppress acid production and allow the esophageal lining to heal. Long-term use of PPIs should be discussed with a doctor, as they can have potential side effects. – Surgery: In rare cases, surgery may be necessary to strengthen the LES or prevent reflux. Fundoplication is a common surgical procedure that wraps part of the stomach around the lower esophagus to tighten the sphincter and reduce acid reflux. Additionally, understanding eating during stress can help you make better choices for your overall health.
In conclusion, chronic heartburn isn’t simply an inconvenience; it’s a signal that your esophagus is under stress and potentially undergoing significant changes. Understanding these changes – from inflammation and metaplasia to Barrett’s esophagus and cancer risk – empowers you to take proactive steps towards protecting your esophageal health. Combining lifestyle modifications, appropriate medical interventions, and regular monitoring can help manage symptoms, prevent complications, and ensure a better quality of life. Early detection and consistent management are key. Remember that this information is for educational purposes only and should not be considered medical advice; always consult with a healthcare professional for diagnosis and treatment of any health condition.