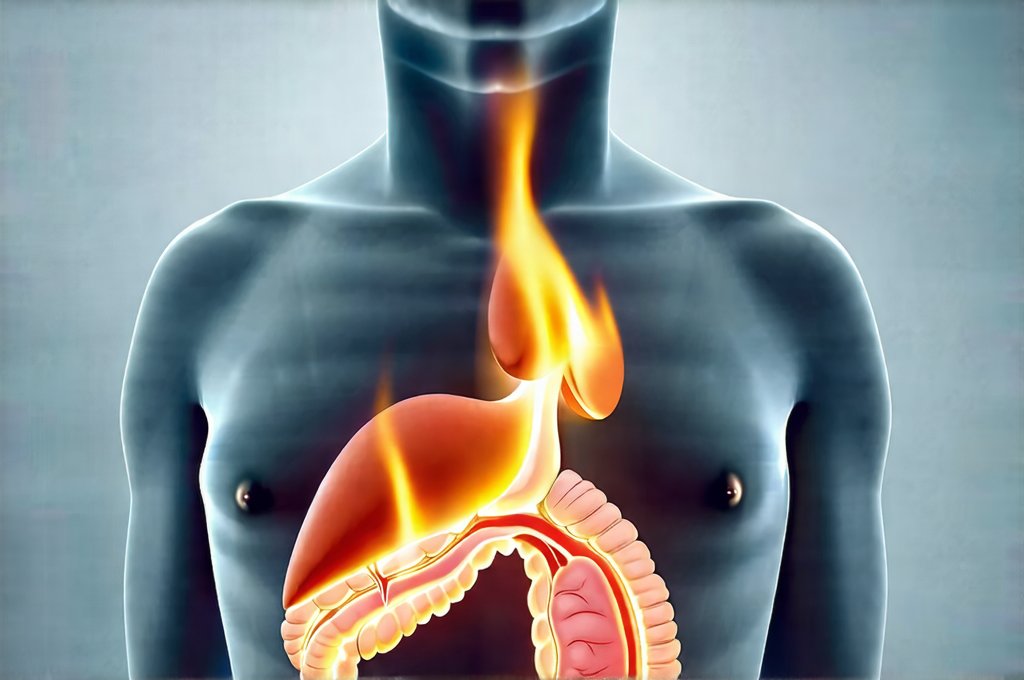
That unsettling burning sensation in your esophagus, seemingly appearing out of nowhere – even when you haven’t eaten anything triggering – can be deeply concerning. It’s a common experience, one many people attribute to heartburn or acid reflux, but the causes are often far more nuanced and complex than simply “too much spice” or an upset stomach. Understanding what might be happening inside your body when this occurs is the first step toward addressing it effectively, and potentially identifying whether further investigation is needed. This isn’t just about discomfort; it’s about recognizing signals your digestive system is sending and responding appropriately.
The feeling can range from a mild warmth to an intense, fiery pain that radiates up into your chest, sometimes even mimicking the symptoms of a heart attack. It’s crucial to differentiate between occasional, short-lived burning sensations and persistent or severe episodes. While isolated instances are usually manageable with over-the-counter remedies or lifestyle adjustments, frequent or debilitating discomfort warrants professional medical attention. Ignoring these signals could allow underlying conditions to worsen or go undiagnosed, impacting your overall health and well-being. This article will explore the common and less common causes of that burning feeling, offering insights into possible explanations and highlighting when it’s time to seek a doctor’s advice.
Gastroesophageal Reflux Disease (GERD) & Acid Reflux
Gastroesophageal reflux disease, or GERD, is arguably the most frequent culprit behind unexplained burning sensations. It happens when stomach acid frequently flows back up into the esophagus – the tube connecting your mouth to your stomach. This backflow, known as acid reflux, irritates the lining of the esophagus, causing that familiar burning feeling often referred to as heartburn. While occasional acid reflux is normal (and many experience it after a large meal), GERD signifies a chronic condition with more frequent and severe symptoms. Several factors contribute to GERD:
- A weakened lower esophageal sphincter (LES): This muscle acts like a valve, preventing stomach contents from flowing back up.
- Hiatal hernia: A portion of the stomach protrudes through the diaphragm, potentially weakening the LES.
- Obesity: Excess weight can put pressure on the abdomen, forcing acid upwards.
- Certain foods and beverages: Spicy foods, fatty foods, caffeine, chocolate, and alcohol can all trigger reflux.
- Smoking: Weakens the LES and increases stomach acid production.
Beyond heartburn, GERD can manifest in other ways, including regurgitation (a sour taste in your mouth), difficulty swallowing, chronic cough, and even asthma-like symptoms. The burning sensation isn’t always directly after eating; it can occur hours later, especially if you lie down soon after a meal or have consumed triggering foods. It’s important to note that lifestyle modifications are often the first line of defense against GERD: elevating the head of your bed, avoiding late-night meals, and identifying/eliminating trigger foods are all beneficial steps.
However, untreated GERD can lead to more serious complications like esophagitis (inflammation of the esophagus), Barrett’s esophagus (a precancerous condition), and esophageal strictures (narrowing of the esophagus). That’s why consistent or worsening symptoms should be evaluated by a physician. There are also medications available, ranging from antacids to proton pump inhibitors (PPIs), that can help manage GERD symptoms and prevent complications. Understanding eating habits is crucial for managing this condition.
Other Digestive Disorders Contributing to Burning Sensations
The burning sensation isn’t always solely attributable to acid reflux. Several other digestive disorders can mimic or exacerbate these feelings. Esophagitis, as mentioned earlier, is inflammation of the esophagus, but it doesn’t always stem from GERD. It can also be caused by infections (bacterial, viral, fungal), allergies, certain medications, or even radiation therapy. The symptoms are similar to heartburn, but may include painful swallowing and a sensation of food getting stuck in your throat.
Another possibility is Peptic Ulcer Disease. While typically associated with stomach pain, ulcers – sores that develop on the lining of the stomach, esophagus, or small intestine – can also cause burning sensations higher up in the digestive tract. These sensations might not always be directly linked to eating, but can worsen after meals, particularly if you have a duodenal ulcer (an ulcer in the first part of the small intestine). The primary causes are often long-term use of NSAIDs or infection with Helicobacter pylori bacteria. If symptoms persist, it may indicate something more serious like acute pancreatitis.
Finally, conditions like Achalasia, where the LES fails to relax properly allowing food to pass into the stomach, can lead to food accumulating in the esophagus and causing a burning sensation due to fermentation and pressure. This is less common than GERD but requires specific medical attention as it obstructs normal digestion. Diagnosis often involves endoscopic examination and motility testing to assess esophageal function. If you experience discomfort after eating, understanding what helps your stomach can provide relief.
Beyond the Digestive System: Non-Digestive Causes
It’s easy to assume the burning sensation originates within your digestive system, but sometimes the source is elsewhere. Cardiac issues, specifically angina or even a heart attack, can present with chest pain that closely resembles heartburn. This is why it’s vital to rule out cardiac causes if you experience new or worsening chest discomfort, especially if accompanied by shortness of breath, sweating, nausea, or pain radiating to your arm or jaw. Never self-diagnose; seek immediate medical attention if you suspect a heart problem.
Another often overlooked cause is esophageal spasm. These painful contractions of the esophageal muscles can feel like intense burning or squeezing and are not related to acid reflux. The exact cause isn’t always known, but stress, extreme temperatures, and certain foods may trigger them.
Furthermore, anxiety and stress can significantly impact digestive function and even create physical sensations mimicking heartburn. The connection between mind and gut is powerful; chronic stress can lead to increased stomach acid production, heightened sensitivity to pain, and altered esophageal motility. While addressing the underlying emotional factors won’t always eliminate the burning sensation, managing stress through techniques like mindfulness, yoga, or therapy can often provide relief. It’s also worth considering that some medications – particularly those taken for other conditions – can have side effects that include esophageal irritation or acid reflux. When you notice frequent discomfort, a belly rub may be telling you something important. If you are experiencing issues with bowel movements, consider looking into constipation relief. Finally, if the burning sensation is accompanied by other symptoms, it may be a sign of gastritis.
Ultimately, pinpointing the exact cause of a persistent burning sensation requires careful evaluation and potentially diagnostic testing conducted by a healthcare professional. Don’t hesitate to seek their guidance if the discomfort is frequent, severe, or accompanied by other concerning symptoms.