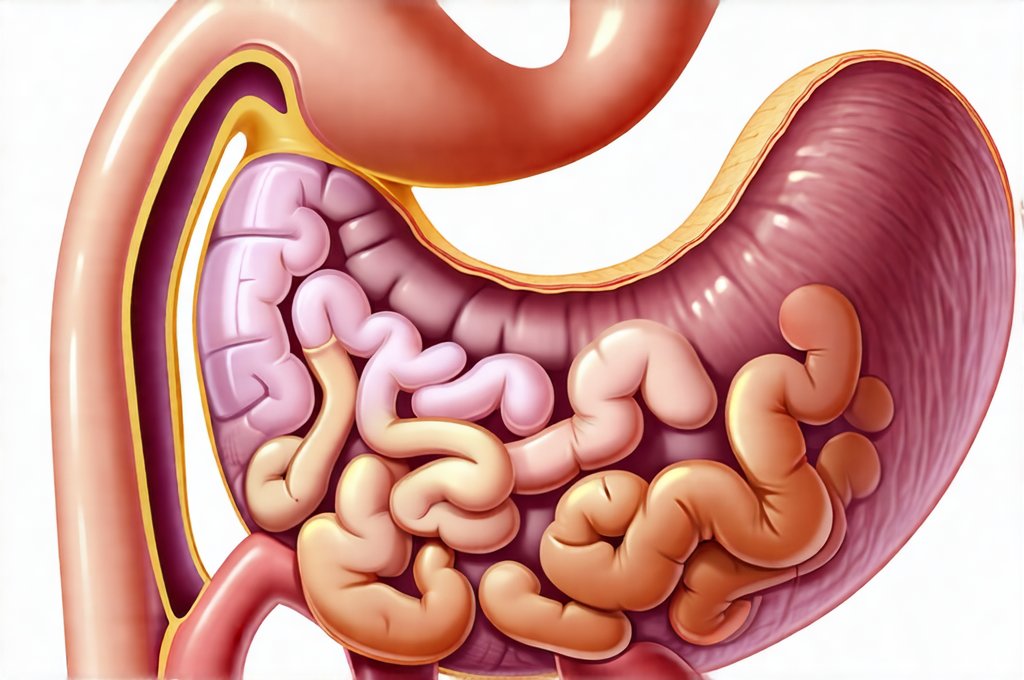
Digestive issues are remarkably common, affecting a significant portion of the population at some point in their lives. From occasional bloating and discomfort to more persistent problems like abdominal pain, nausea, and changes in bowel habits, these symptoms can significantly impact quality of life. Many anxieties surrounding digestive complaints stem from the fear of serious underlying conditions – things like inflammatory bowel disease, cancer, or structural abnormalities. Fortunately, a range of sophisticated imaging techniques are available to help healthcare professionals accurately diagnose the cause of digestive distress and, crucially, rule out more severe possibilities, providing reassurance and guiding appropriate treatment strategies. Understanding these tools empowers patients to actively participate in their care and approach health concerns with informed confidence.
The process of investigating digestive symptoms often begins with a thorough medical history and physical examination. However, when symptoms are persistent or raise red flags, imaging tests become invaluable. These tests don’t just detect problems; they offer detailed visualizations that allow clinicians to pinpoint the location, size, and nature of any abnormalities. The choice of imaging modality depends heavily on the specific symptoms, suspected diagnosis, and patient factors like age, overall health, and potential risks associated with the test itself. It’s important to remember that imaging is typically one piece of a larger diagnostic puzzle, often used in conjunction with other tests such as blood work, stool analysis, and endoscopy/colonoscopy. Considering comfort-based food routines can also be beneficial during this process.
The Role of X-Rays and Computed Tomography (CT) Scans
X-rays have long been a cornerstone of medical diagnostics, and while they are less frequently the first line for complex digestive investigations today, they still play a role, particularly in emergency situations or initial assessments. A basic abdominal x-ray can quickly identify blockages, perforations (holes), or large masses. However, x-rays provide limited detail regarding soft tissues, making them less useful for diagnosing many digestive conditions. CT scans, on the other hand, represent a significant advancement. They utilize x-rays but employ sophisticated computer processing to create cross-sectional images of the body, offering far greater clarity and detail than traditional x-rays.
CT scans are exceptionally helpful in evaluating abdominal pain, identifying sources of infection (like appendicitis or diverticulitis), detecting tumors, assessing inflammatory bowel disease, and visualizing internal bleeding. They can also be used to guide biopsies – procedures where a small tissue sample is taken for further analysis. A key advantage of CT scanning is its speed; scans can often be completed relatively quickly, making them ideal for emergency situations. However, it’s important to acknowledge the radiation exposure associated with CT scans, and clinicians carefully weigh the benefits against the risks, particularly in younger patients or those requiring repeated imaging. Simple ways to upgrade your routine can also help minimize issues that might require such intensive diagnostics.
CT enterography and CT colonography are specialized CT techniques focusing on specific areas of the digestive system. CT Enterography involves drinking a liquid contrast agent that highlights the small intestine, allowing for detailed visualization of its walls and identification of inflammation, tumors, or strictures (narrowings). CT Colonography, often called “virtual colonoscopy,” uses air to inflate the colon and provides images similar to those obtained during a traditional colonoscopy, but without the need for sedation or insertion of an endoscope. It’s primarily used for colorectal cancer screening and detecting polyps. If stress is a factor, explore comfort meals to ease tension.
Utilizing Ultrasound for Digestive Assessment
Ultrasound technology utilizes sound waves to create images of internal organs. It is non-invasive, relatively inexpensive, and does not involve ionizing radiation, making it a safe and readily available imaging option. While ultrasound isn’t as penetrating as CT scans or MRI, it’s incredibly useful for evaluating certain digestive concerns.
- Specifically, gallbladder disease (gallstones, inflammation) is often diagnosed with ultrasound due to its high accuracy in detecting these conditions.
- Ultrasound can also assess the liver, pancreas, and kidneys, identifying abnormalities like cysts, tumors, or fluid collections.
- Endoscopic ultrasound (EUS) combines endoscopy – inserting a flexible tube with a camera into the digestive tract – with ultrasound technology. This allows for detailed imaging of the esophagus, stomach, duodenum, pancreas, and bile ducts from within the body. EUS is particularly valuable in diagnosing pancreatic cancer, evaluating unexplained abdominal pain, and guiding fine-needle biopsies. Symptoms that point to imbalances should be checked promptly.
The effectiveness of ultrasound depends heavily on operator skill and patient factors like body habitus (size and shape). In obese patients or those with significant bowel gas, obtaining clear images can be more challenging. However, its safety profile and accessibility make it a valuable first step in many digestive investigations. Understanding how to detect subtle issues can improve outcomes.
Magnetic Resonance Imaging (MRI) – A Detailed View
Magnetic resonance imaging (MRI) employs strong magnetic fields and radio waves to create detailed images of internal organs. Unlike x-rays or CT scans, MRI does not use ionizing radiation, making it an attractive option for patients who require repeated imaging or are concerned about radiation exposure. MRI provides exceptional soft tissue contrast, allowing for highly accurate visualization of the digestive system, particularly the liver, pancreas, bile ducts, and bowel.
MRI is often used to evaluate:
– Complex cases of inflammatory bowel disease (Crohn’s disease and ulcerative colitis), where it can identify areas of inflammation, strictures, or fistulas (abnormal connections between organs).
– Liver tumors and other liver abnormalities with great precision.
– Bile duct disorders like gallstones or blockages.
– Perianal diseases – conditions affecting the area around the anus.
One limitation of MRI is its longer scan time compared to CT scans, which can be challenging for patients who are claustrophobic or unable to remain still for extended periods. Additionally, metal implants can interfere with image quality and may preclude the use of MRI in some individuals. MR enterography and MR cholangiopancreatography (MRCP) are specialized MRI techniques that provide detailed views of the small intestine and biliary/pancreatic system respectively. Supporting digestive health through digestive support foods can complement diagnostic efforts. Using movement to stimulate digestive flow is also a helpful habit.
The information provided here is intended for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.