The intricate relationship between our gut microbiota—the trillions of microorganisms residing in our digestive tract—and overall health is rapidly becoming one of the most exciting areas of modern scientific inquiry. For decades, we’ve understood that diet plays a crucial role in maintaining well-being, but now we’re realizing it’s not just what we eat, but how our individual gut ecosystems respond to those foods that truly matters. This realization has paved the way for personalized nutrition, moving beyond generalized dietary recommendations toward plans tailored to an individual’s unique microbial profile. Gut microbiota testing is emerging as a powerful tool in this shift, offering insights into the composition and function of these communities and enabling more targeted nutritional interventions.
Traditionally, nutritional advice often followed a “one-size-fits-all” approach. However, people respond differently to the same foods due to variations in genetics, lifestyle, and crucially, their gut microbiota. This diversity impacts everything from nutrient absorption and immune function to mental health and even chronic disease risk. The gut microbiome influences digestion, synthesizes vitamins (like K and some B vitamins), modulates inflammation, and protects against pathogens. Understanding its individual characteristics is therefore key to optimizing health. Gut testing isn’t about identifying “good” or “bad” bacteria in isolation; it’s about assessing the balance of microbial communities and their functional capabilities.
The Science Behind Gut Microbiota Testing
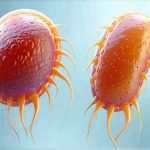
Gut microbiota testing aims to characterize the complex ecosystem within your digestive tract, moving beyond simple identification of bacterial species to reveal insights into their collective function. Several technologies are employed, but the most common relies on analyzing microbial DNA extracted from a stool sample – though breath and urine tests are also gaining traction. These tests typically employ 16S rRNA gene sequencing or shotgun metagenomic sequencing. 16S rRNA gene sequencing identifies bacteria based on a specific gene sequence present in all bacteria, providing information about the types of microbes present but limited insight into their functions. Shotgun metagenomic sequencing, on the other hand, sequences all the DNA in a sample, offering a more comprehensive picture including microbial function (what genes they express) and metabolic pathways.
The data generated from these tests isn’t simply a list of bacteria names. Advanced analysis techniques are used to interpret the results, often comparing an individual’s microbiome against reference ranges or established healthy profiles. This allows for identification of potential imbalances – dysbiosis – or deficiencies in beneficial microbes. It’s important to note that interpreting gut testing data requires expertise. A diverse and abundant microbiome isn’t necessarily “better” than a less diverse one; the functional capacity of the microbiota is what truly matters. Factors such as diet, antibiotic use, stress levels, and geographical location all significantly impact microbial composition, making individual interpretation vital.
The ongoing evolution of testing methodologies means that accuracy and precision are continually improving. While earlier tests faced limitations in identifying certain microbes or accurately assessing functional potential, advancements in sequencing technology and bioinformatics analysis are providing increasingly reliable and detailed results. However, it’s crucial to approach these tests with a critical eye; they provide valuable information, but aren’t definitive diagnoses or predictors of health outcomes on their own. They serve best as part of a broader assessment alongside clinical evaluation and lifestyle factors. Consider also how testing guides personal nutrition for more personalized plans.
Translating Test Results into Actionable Nutrition Plans
Once gut microbiota testing is completed, the real work begins: translating the data into personalized nutritional recommendations. This isn’t about eliminating entire food groups or adhering to rigid diets; it’s about strategically adjusting dietary patterns to support a healthier microbiome and optimize individual responses. A skilled practitioner – often a registered dietitian specializing in gut health or a functional medicine physician – will review the test results, considering them within the context of your overall health history, symptoms, and lifestyle factors.
The focus isn’t solely on increasing “good” bacteria; it’s about fostering microbial diversity and balance. This might involve strategies to: – Increase fiber intake to feed beneficial microbes. Different types of fiber support different species, so variety is key. – Incorporate fermented foods like yogurt, kefir, sauerkraut, and kimchi, which introduce live probiotics (beneficial bacteria) into the gut. – Reduce processed foods, sugar, and artificial sweeteners, as these can negatively impact microbial composition. – Identify potential food sensitivities or intolerances that may be contributing to inflammation or dysbiosis. – Address nutrient deficiencies identified through testing or clinical assessment. It’s helpful to learn using test results when adjusting diet.
Personalized nutrition plans based on gut microbiota testing often emphasize prebiotics – non-digestible fibers that selectively feed beneficial bacteria in the colon. Different prebiotics support different microbial populations, so a tailored approach is vital. For example, individuals with low levels of Bifidobacteria might benefit from foods rich in galacto-oligosaccharides (GOS), found in legumes and onions, while those aiming to increase Akkermansia muciniphila—a bacterium associated with improved metabolic health – may focus on polyphenols found in berries, cocoa, and green tea. It’s also important to remember that dietary changes should be gradual and sustainable, avoiding drastic restrictions that can further disrupt the microbiome. Balanced nutrition plans are key here.
The Role of Fiber & Resistant Starch
Fiber is arguably the cornerstone of a healthy gut microbiome. It’s not digested by our own enzymes, allowing it to reach the colon where it’s fermented by microbial communities. This fermentation process produces short-chain fatty acids (SCFAs) – such as butyrate, propionate, and acetate – which are crucial for gut health and overall well-being. Butyrate, in particular, is a primary energy source for colon cells and possesses anti-inflammatory properties. Different types of fiber support different microbial populations, highlighting the importance of dietary diversity.
Resistant starch, another type of indigestible carbohydrate, behaves similarly to fiber and plays a significant role in promoting gut health. It’s found in foods like cooked and cooled potatoes, green bananas, oats, and legumes. Resistant starch resists digestion in the small intestine, reaching the colon where it’s fermented by bacteria, also producing SCFAs. Incorporating resistant starch into your diet can help improve insulin sensitivity, reduce inflammation, and enhance gut barrier function. However, increasing fiber intake too quickly can lead to bloating and discomfort; gradual increases are recommended alongside adequate hydration. You may want to consider gentle cooking methods to maximize nutrient absorption.
The interplay between fiber type, microbial composition, and SCFA production is complex and individual. Gut microbiota testing can provide valuable insights into which types of fiber might be most beneficial for a particular person based on their microbial profile. For example, individuals with low levels of bacteria capable of fermenting certain fibers may need to focus on alternative sources or slowly introduce those fibers to allow the microbiome to adapt.
Addressing Dysbiosis & Inflammation
Dysbiosis – an imbalance in the gut microbial community – is often linked to various health issues, including digestive disorders, autoimmune diseases, and mental health conditions. Gut microbiota testing can help identify specific imbalances, such as a reduction in beneficial bacteria or an overgrowth of potentially harmful species. Addressing dysbiosis typically involves dietary modifications aimed at restoring balance. This may include increasing fiber intake, incorporating fermented foods, reducing sugar and processed food consumption, and addressing any identified nutrient deficiencies.
Chronic inflammation is frequently associated with gut dysbiosis. The microbiome plays a vital role in modulating the immune system, and imbalances can contribute to increased intestinal permeability – often referred to as “leaky gut” – allowing inflammatory molecules to enter the bloodstream. Dietary strategies aimed at reducing inflammation include incorporating anti-inflammatory foods rich in omega-3 fatty acids (like salmon and flaxseeds), polyphenols (found in berries and green tea), and probiotics (from fermented foods).
Identifying food sensitivities or intolerances can also be crucial in addressing gut inflammation. Gut microbiota testing doesn’t directly identify food allergies, but it can sometimes reveal clues about potential triggers based on microbial imbalances. An elimination diet – guided by a healthcare professional – may be recommended to identify and remove problematic foods, allowing the gut to heal and reduce inflammation. Testing for inflammation can help pinpoint causes of discomfort.
The Future of Personalized Nutrition & Microbiome Testing
Gut microbiota testing is still a relatively new field, but it’s evolving rapidly. Advances in sequencing technology and bioinformatics are leading to more accurate and detailed assessments of microbial composition and function. Future developments may include: – More sophisticated tests capable of assessing the virome (viral communities within the gut) and mycobiome (fungal communities). – Integration of microbiome data with other “omics” technologies, such as genomics, proteomics, and metabolomics, to provide a more holistic understanding of individual health. – Development of AI-powered algorithms capable of predicting an individual’s response to specific dietary interventions based on their microbial profile.
The increasing accessibility and affordability of gut microbiota testing are also contributing to its growing popularity. However, it’s essential to remember that these tests are just one piece of the puzzle. They should be used in conjunction with clinical evaluation, lifestyle assessments, and personalized guidance from a qualified healthcare professional. The future of nutrition is undeniably moving toward personalization, and gut microbiota testing will continue to play a central role in unlocking the secrets of our individual microbial ecosystems and optimizing health for years to come. It’s not just about changing what we eat; it’s about understanding how our unique microbiomes respond to those choices and tailoring our diets accordingly. How testing guides nutrition is becoming more widespread as the science advances, and GI tests guide supplement plans.