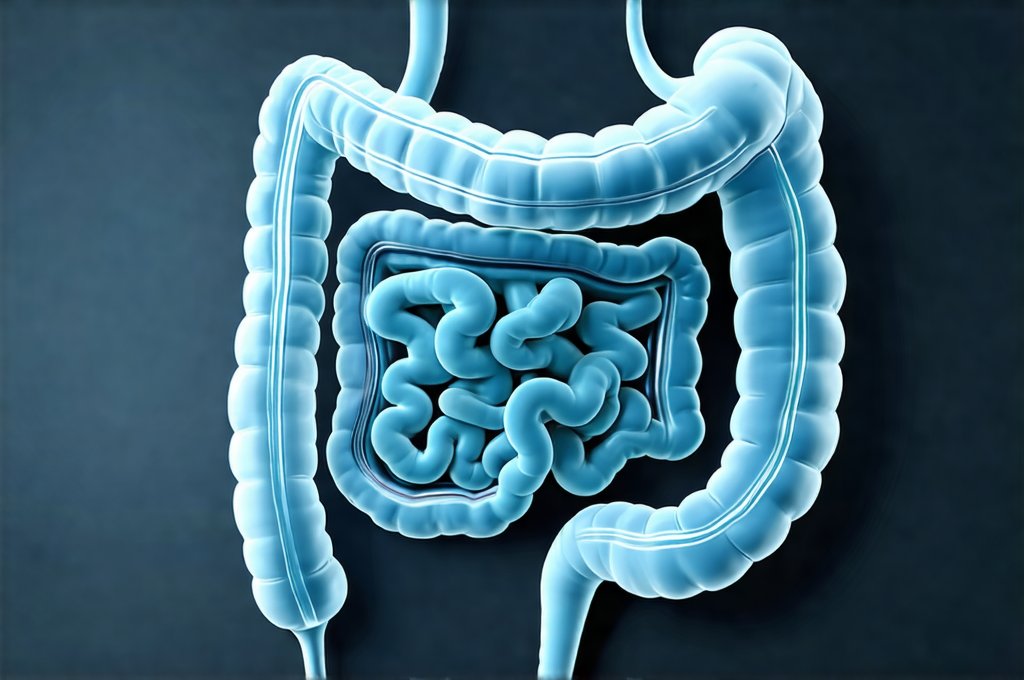
The gut – often referred to as our “second brain” – is far more than just a digestive tract. It’s an incredibly complex ecosystem influencing everything from nutrient absorption and immune function to mental wellbeing and even chronic disease risk. For many, understanding their gut health feels daunting, inextricably linked to invasive procedures like colonoscopies. However, a surprisingly detailed assessment of your gut’s functionality can be achieved without subjecting yourself to such interventions. This exploration delves into accessible methods for gaining insights into your digestive system, identifying potential imbalances, and supporting optimal gut health through lifestyle adjustments and mindful observation.
We often perceive gut health as something only relevant when problems arise – bloating, constipation, or more severe issues. But proactively understanding your gut is about preventative care, building resilience against future ailments, and maximizing overall vitality. It’s about recognizing the subtle signals our bodies send us and responding with informed choices. This isn’t simply about eliminating foods; it’s about cultivating a thriving internal environment where beneficial bacteria flourish and digestion operates smoothly. A healthy gut contributes significantly to energy levels, mood regulation, and even the effectiveness of medications we might take – making it an area worthy of focused attention. If you suspect your microbiome is off, consider looking at signs that your health needs a boost.
Decoding Your Digestive Signals
Our bodies are constantly communicating with us, often through seemingly minor signals that we dismiss or attribute to other causes. Learning to ‘listen’ to your gut is the first step in understanding its state. This isn’t about self-diagnosing; it’s about becoming more attuned to how different foods and lifestyle factors impact your digestive process. Pay close attention to regularity, consistency, and any associated discomfort. – Is your bowel movement predictable? – What does it look like – color, form, presence of undigested food? – Do you experience gas, bloating, cramping, or heartburn after eating certain foods? Keeping a detailed food diary alongside symptom tracking can reveal patterns that might otherwise go unnoticed. If you find yourself needing to reset your gut after overindulging, there are steps you can take.
The Bristol Stool Chart is an incredibly useful tool for objectively assessing stool consistency. It categorizes bowel movements on a scale of 1 to 7, ranging from hard, separate lumps (Type 1 – constipation) to watery stools (Type 7 – diarrhea). Regularly checking your stool against this chart provides valuable data that can help identify imbalances. Furthermore, observing the timing between meals and subsequent digestive responses is crucial. Food intolerances or sensitivities often manifest as delayed digestion, leading to bloating or discomfort hours after eating. It’s important to remember that individual experiences vary greatly; what’s ‘normal’ for one person isn’t necessarily normal for another. Understanding what to eat on busy days can help prevent issues as well.
A key aspect of decoding your gut signals lies in recognizing the difference between acute and chronic issues. Occasional digestive upset is common – perhaps from a particularly rich meal or a stressful event. However, persistent symptoms warrant further investigation with a healthcare professional. The goal here isn’t to become an expert diagnostician but rather an informed observer of your body’s unique responses, empowering you to make proactive lifestyle adjustments and communicate effectively with your doctor when needed.
Exploring Non-Invasive Testing Options
While colonoscopies provide detailed visual assessment, several non-invasive tests offer valuable insights into gut health without requiring such procedures. Stool testing is arguably the most accessible option. These tests can analyze various markers in your stool, including: – Calprotectin levels (indicating inflammation) – Fecal Immunochemical Test (FIT) for hidden blood – a screening tool for colorectal cancer, but also indicative of potential gut irritation. – Microbiome analysis (identifying the composition of bacteria in your gut). While microbiome tests are becoming increasingly popular, their interpretation can be complex and should ideally be discussed with a healthcare professional.
Another option is breath testing, particularly useful for identifying Small Intestinal Bacterial Overgrowth (SIBO). This test measures hydrogen and methane levels in your breath after consuming a specific sugar solution. Elevated levels suggest bacterial fermentation occurring higher up in the digestive tract than it should, potentially leading to bloating, gas, and malabsorption. It’s crucial to understand that these tests aren’t replacements for colonoscopies when screening for colorectal cancer or other serious conditions. They provide complementary information about gut function rather than structural abnormalities. If you are planning a trip, consider how to travel without triggering your gut.
Finally, consider food sensitivity testing (though its scientific validity remains debated). These tests typically involve eliminating certain foods from your diet and then reintroducing them one by one, observing any associated symptoms. While not a definitive diagnostic tool, it can help identify potential triggers for digestive discomfort. It’s vital to approach all non-invasive testing with caution and interpret results in consultation with a healthcare professional who can provide personalized guidance. Why some days your gut feels off is often complex, so seeking advice is useful.
Lifestyle Adjustments for Gut Health
Beyond testing, actively supporting your gut health through lifestyle modifications is paramount. Diet plays a central role. Increasing fiber intake – from fruits, vegetables, whole grains, and legumes – provides fuel for beneficial bacteria and promotes regularity. Conversely, reducing processed foods, sugary drinks, and excessive amounts of red meat can minimize inflammation and support a healthy microbiome. Incorporating fermented foods like yogurt, kefir, sauerkraut, and kimchi introduces probiotics (live microorganisms) that contribute to gut diversity.
Stress management is often overlooked but profoundly impacts gut health. Chronic stress disrupts the delicate balance of the gut microbiome and can exacerbate digestive symptoms. Techniques like mindfulness meditation, yoga, deep breathing exercises, and regular physical activity can help mitigate stress levels and promote a calmer digestive system. Equally important is adequate sleep. Lack of sleep has been linked to changes in gut bacteria composition and increased intestinal permeability (often referred to as “leaky gut”). It’s also helpful to understand why your gut might feel like a balloon after stress.
Hydration is also crucial for optimal digestion. Water helps move food through the digestive tract, preventing constipation and supporting nutrient absorption. Aim for at least eight glasses of water per day, adjusting based on activity level and climate. Prioritizing these lifestyle adjustments can significantly improve gut health even without specific diagnostic testing – it’s about creating a supportive internal environment that allows your digestive system to thrive. Remember consistency is key; small, sustainable changes are more effective than drastic, short-lived interventions. Eating out doesn’t have to stress your gut – learn how to eat without worry.