Gas, bloating, and flatulence are incredibly common experiences, often causing discomfort but rarely signaling a serious underlying condition. Most people experience these symptoms occasionally, usually related to diet or lifestyle factors. However, when these symptoms become persistent, excessive, or accompanied by other concerning signs, it’s important to understand the potential causes and available diagnostic approaches. This article will explore typical diagnostics used to investigate gas, bloating, and flatulence, focusing on how healthcare professionals approach identifying the root cause of these often-uncomfortable issues. It’s crucial to remember that self-diagnosis can be misleading; a proper evaluation by a medical professional is always recommended when symptoms are bothersome or persistent.
The experience of gas, bloating, and flatulence varies greatly from person to person. Some individuals may notice mild discomfort after eating certain foods, while others might experience debilitating pain and significant social anxiety due to excessive gas production. Understanding the difference between normal physiological occurrences and potential medical concerns is key to appropriate diagnosis and management. Often, simple dietary adjustments can alleviate symptoms, but identifying food sensitivities or underlying digestive disorders requires a more thorough investigation using various diagnostic tools. It’s also important to differentiate between acute episodes of bloating (often related to a single meal) and chronic bloating which may indicate an ongoing issue requiring medical attention.
Initial Assessment & Patient History
The first step in diagnosing the cause of gas, bloating, and flatulence is a comprehensive assessment by a healthcare provider. This typically begins with a detailed patient history, focusing on symptom characteristics and potential contributing factors. The doctor will ask about: – Frequency and duration of symptoms – When did they start? How often do they occur? How long do they last? – Severity of symptoms – On a scale of 1-10, how disruptive are these symptoms to daily life? – Specific triggers – Are there certain foods, activities, or times of day that seem to worsen symptoms? – Associated symptoms – Are there any accompanying symptoms like abdominal pain, diarrhea, constipation, nausea, weight loss, or fatigue? – Medical history – Do you have any pre-existing medical conditions, such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), celiac disease, or lactose intolerance? – Medication and supplement use – Are you taking any medications or supplements that could potentially contribute to these symptoms? – Dietary habits – What is your typical diet like? Do you consume a lot of gas-producing foods, such as beans, broccoli, cabbage, onions, or carbonated beverages?
This initial interview helps the healthcare professional narrow down potential causes and guide further diagnostic testing. A thorough understanding of the patient’s lifestyle and medical background is essential for accurate diagnosis. Often, simply identifying dietary patterns or medication side effects can explain the symptoms without requiring extensive testing. The doctor may also perform a physical examination, including palpating the abdomen to check for tenderness, distension, or masses. This helps rule out more serious conditions and provides additional clues about the underlying cause of the symptoms. Considering creative wraps and bowls can also help manage dietary intake.
Diagnostic Testing Options
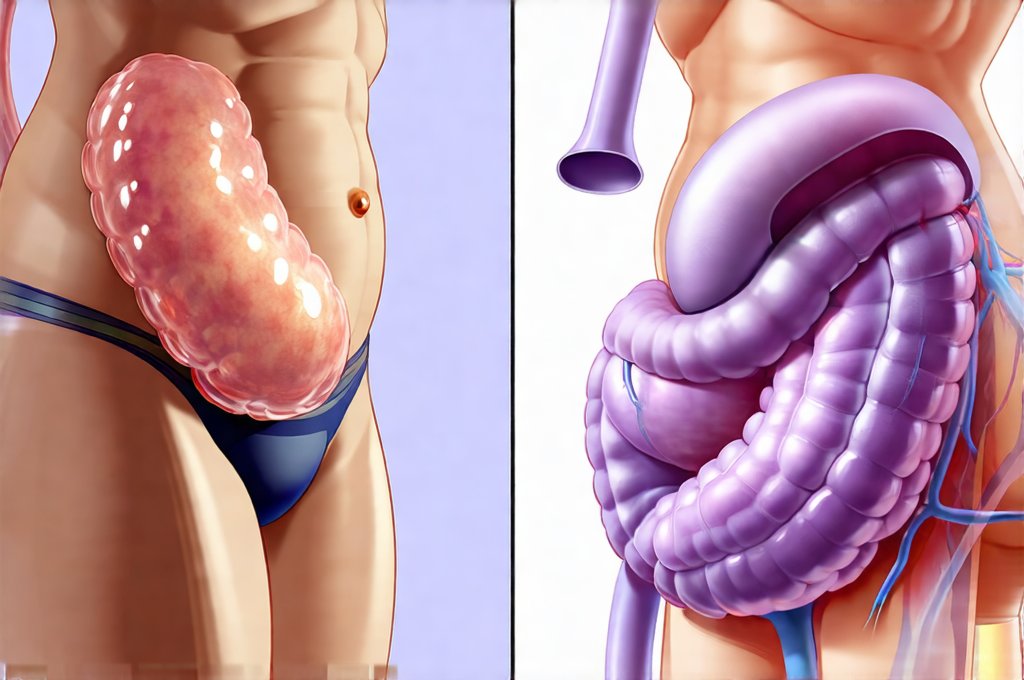
Depending on the information gathered during the initial assessment, various diagnostic tests might be recommended. These tests aim to identify specific causes of gas, bloating, and flatulence, ranging from food intolerances to digestive disorders. Common testing options include: – Hydrogen breath test: This test is used to diagnose lactose intolerance, fructose malabsorption, and small intestinal bacterial overgrowth (SIBO). It measures the amount of hydrogen gas exhaled after consuming a specific sugar solution. Elevated hydrogen levels indicate that the body is not properly digesting the sugar. – Stool tests: These tests can help identify infections, parasites, or malabsorption issues. They may also assess for fecal calprotectin, a marker of inflammation in the digestive tract. – Blood tests: Blood tests can rule out celiac disease (through antibody testing), check for anemia, and assess overall health markers. – Endoscopy/Colonoscopy: While less common for initial investigations of gas and bloating, these procedures may be recommended if more serious conditions are suspected or if other tests yield inconclusive results. They allow direct visualization of the digestive tract to identify inflammation, ulcers, or tumors.
It’s important to note that not every patient will require all of these tests. The healthcare provider will select the most appropriate tests based on the individual’s symptoms, medical history, and physical examination findings. The goal is to pinpoint the underlying cause of the symptoms in the least invasive way possible. Often, a combination of testing and dietary adjustments are used to arrive at an accurate diagnosis. Implementing mini fasts can support digestive recovery during these tests.
Food Intolerance & Elimination Diets
Food intolerances play a significant role in many cases of gas, bloating, and flatulence. Unlike food allergies which involve an immune response, food intolerances occur when the body has difficulty digesting certain foods. Common culprits include lactose (in dairy products), fructose (in fruits and honey), gluten (in wheat, barley, and rye), and FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols). Diagnosing food intolerance often involves an elimination diet, where suspected trigger foods are removed from the diet for a period of time.
The elimination phase typically lasts several weeks, during which the patient carefully monitors their symptoms. After eliminating potential triggers, foods are reintroduced one at a time to observe any reactions. This process helps identify specific foods that contribute to gas, bloating, or other digestive issues. It’s crucial to work with a registered dietitian when following an elimination diet to ensure adequate nutritional intake and proper guidance on reintroduction strategies. Hydrogen breath tests can also be used to confirm lactose intolerance or fructose malabsorption as mentioned previously. Understanding the connection between food combining is useful during this process.
Small Intestinal Bacterial Overgrowth (SIBO)
Small intestinal bacterial overgrowth (SIBO) occurs when there is an excessive amount of bacteria in the small intestine. This can lead to fermentation of undigested carbohydrates, resulting in gas production, bloating, and abdominal discomfort. Diagnosing SIBO typically involves a hydrogen breath test, similar to those used for lactose intolerance or fructose malabsorption. However, in this case, the patient is given a glucose solution, and the amount of hydrogen and methane produced by bacteria is measured over several hours.
Elevated levels of hydrogen and/or methane suggest bacterial overgrowth. Treatment for SIBO often involves antibiotics to reduce the bacterial population, followed by dietary modifications to prevent recurrence. It’s important to address any underlying factors that may contribute to SIBO, such as motility issues or structural abnormalities in the digestive tract. SIBO can be difficult to diagnose and manage effectively, so working with a gastroenterologist is often recommended. Utilizing balanced sauces during dietary modifications can help ensure palatable meals.
Irritable Bowel Syndrome (IBS) & Other Functional Disorders
Irritable bowel syndrome (IBS) is a common functional gastrointestinal disorder characterized by abdominal pain, bloating, gas, diarrhea, and/or constipation. Unlike inflammatory bowel disease (IBD), IBS does not cause inflammation or damage to the digestive tract. Diagnosis of IBS typically relies on symptom criteria established by the Rome IV guidelines. These guidelines emphasize the presence of recurrent abdominal pain at least one day per week for the past three months, along with two or more of the following: – Relief with defecation – Change in stool frequency – Change in stool appearance
There is no single test to diagnose IBS; instead, healthcare professionals use a process of exclusion to rule out other potential causes. This often involves blood tests, stool tests, and potentially colonoscopy. Other functional gastrointestinal disorders, such as functional dyspepsia (indigestion) can also cause similar symptoms. Management of IBS typically involves dietary modifications, stress management techniques, and sometimes medication to alleviate specific symptoms. A multidisciplinary approach involving a gastroenterologist, registered dietitian, and mental health professional is often beneficial for individuals with IBS. Incorporating self-massage techniques can provide additional relief and improve digestive circulation. Consider also exploring gut-safe sauces to support your diet. Finally, tailored meal plans can provide structure and promote digestive health.