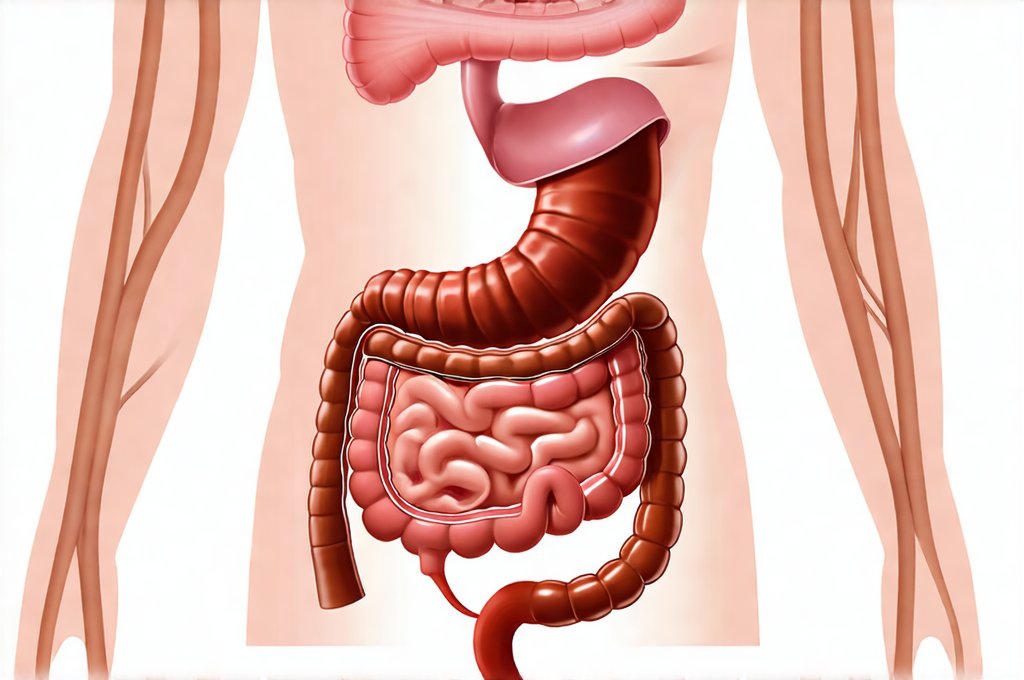
Silent inflammation within the digestive tract is often a hidden culprit behind a wide range of seemingly unrelated symptoms. Unlike acute inflammation – which presents with obvious signs like pain, redness, and swelling – silent inflammation smolders beneath the surface, gradually eroding gut health and potentially contributing to systemic issues over time. This insidious process can be particularly challenging to identify because its symptoms are frequently vague or attributed to other causes, leading to delayed diagnosis and appropriate intervention. Many individuals may experience bloating, fatigue, food sensitivities, or even mood disturbances without realizing these could stem from chronic low-grade inflammation within their digestive system.
Understanding the nuances of gut inflammation is crucial for proactive health management. The gut microbiome plays a central role; imbalances (dysbiosis) can trigger an immune response and perpetuate inflammatory cycles. Lifestyle factors such as diet, stress levels, sleep quality, and exposure to environmental toxins further influence this delicate ecosystem. Identifying silent inflammation isn’t necessarily about pinpointing a single cause, but rather recognizing the patterns and markers that suggest it’s occurring. This requires a multi-faceted approach utilizing both clinical assessment and targeted testing options designed to reveal subtle indicators of gut dysfunction. It is important to remember that these tools provide information, not definitive diagnoses; interpretation should always be done by a qualified healthcare professional. Considering foods that satisfy can also support gut health.
Diagnostic Tools & Approaches
The complexity of silent inflammation necessitates a comprehensive diagnostic strategy. Traditional methods often fall short in detecting low-grade inflammation because they typically focus on acute markers like C-reactive protein (CRP) which spikes during active infections or injury. For gut-specific assessment, we need tools that delve deeper into the intestinal environment and immune responses. Stool testing has emerged as a powerful starting point, offering insights into microbiome composition, inflammatory markers like calprotectin (a marker of neutrophil activity in the gut), and digestive function. However, it’s vital to choose reputable labs utilizing advanced sequencing technologies for accurate results. Beyond stool analysis, breath tests can help identify Small Intestinal Bacterial Overgrowth (SIBO) – a condition often associated with inflammation – and food intolerance testing, while not always definitive, can guide dietary modifications aimed at reducing gut irritation. You may also want to review digestive support foods for your fridge.
The interpretation of these tests requires expertise. A positive calprotectin result, for example, doesn’t automatically equate to Inflammatory Bowel Disease (IBD); it simply indicates inflammation is present, necessitating further investigation. Similarly, SIBO breath test results should be correlated with clinical symptoms and patient history. Relying solely on test outcomes without considering the broader clinical picture can lead to misdiagnosis or inappropriate treatment strategies. A holistic approach that integrates testing with a detailed medical history, symptom analysis, and dietary assessment is key to accurately identifying and addressing silent inflammation in the digestive tract. Focusing on portion awareness habits can also be beneficial.
The choice of diagnostic tools should also be individualized based on the patient’s specific symptoms and suspected underlying causes. For example, someone experiencing primarily neurological symptoms alongside gut issues might benefit from investigating gut-brain axis dysfunction through more specialized testing focused on intestinal permeability (“leaky gut”) or microbial metabolites impacting brain function. This highlights the importance of working with a healthcare provider knowledgeable about functional medicine or integrative gastroenterology who can tailor the diagnostic process to each patient’s unique needs. Remember that rest days for recovery are also crucial.
Stool Analysis: Unveiling Gut Ecosystems
Stool analysis represents one of the most accessible and informative tools for identifying silent inflammation within the digestive tract. Modern stool tests go far beyond simply checking for pathogens; they now provide detailed insights into the composition of the gut microbiome, levels of beneficial bacteria versus potentially harmful ones, and markers indicative of inflammation.
- Comprehensive Digestive Stool Analysis (CDSA) is a frequently used option, assessing parameters like fecal pH, short-chain fatty acids (SCFAs – indicators of microbial fermentation), pancreatic elastase (a measure of digestive capacity), and immune markers such as calprotectin and secretory IgA (an antibody involved in gut immunity).
- PCR-based stool testing can identify specific bacteria, fungi, and parasites with high accuracy.
- Metagenomic sequencing provides the most detailed picture of microbiome diversity, identifying even low-abundance species and predicting their functional capabilities.
Interpreting these results requires a nuanced understanding of microbial ecology. A decrease in SCFA production, for example, suggests reduced beneficial fermentation, potentially leading to inflammation. Elevated calprotectin levels signal an active immune response within the gut. Low secretory IgA indicates compromised gut immunity, making it more vulnerable to pathogens and inflammatory triggers. It’s also important to remember that microbiome composition varies significantly between individuals; what constitutes a “healthy” microbiome is not universally defined. Dietary choices such as foods for pH balance can support microbial diversity.
Breath Testing: Identifying SIBO & Carbohydrate Malabsorption
Breath testing offers a non-invasive method for assessing gut function, specifically identifying Small Intestinal Bacterial Overgrowth (SIBO) and carbohydrate malabsorption. SIBO occurs when excessive bacteria colonize the small intestine – where they shouldn’t be in large numbers – leading to fermentation of undigested carbohydrates and production of gases like hydrogen and methane.
- The process involves consuming a specific sugar solution (typically lactulose or glucose) and collecting breath samples at regular intervals over several hours.
- Elevated levels of hydrogen, methane, or both in the breath indicate bacterial fermentation occurring higher up in the digestive tract than it should be.
- Different sugars are used to assess different parts of the small intestine; for example, lactulose is less absorbed and tests the entire length, while glucose primarily assesses the proximal small intestine.
Carbohydrate malabsorption can also be identified through breath testing, using substrates like lactose or fructose. In this case, undigested carbohydrates reach the colon where they are fermented by bacteria, leading to gas production. Symptoms associated with SIBO and carbohydrate malabsorption – bloating, abdominal pain, diarrhea, constipation – often overlap, making accurate diagnosis crucial for targeted treatment. It’s important to note that breath tests have limitations; false positives can occur due to factors like rapid gut transit time or recent antibiotic use. Hydrating foods can also support digestive health.
Intestinal Permeability Testing: Assessing “Leaky Gut”
The concept of “leaky gut” – increased intestinal permeability – has gained significant attention in functional medicine. While the term itself is often debated, the underlying principle of compromised intestinal barrier function is well-recognized. A healthy intestinal lining acts as a selective barrier, allowing nutrients to pass through while preventing harmful substances from entering the bloodstream. When this barrier becomes damaged, larger molecules can “leak” into circulation, triggering an immune response and contributing to systemic inflammation.
- Zonulin is a protein that regulates intestinal permeability and can be measured in stool samples as an indicator of barrier dysfunction. Elevated zonulin levels suggest increased permeability.
- Lactulose/Mannitol Ratio (LMR) test assesses gut permeability by measuring the excretion of these two sugars after ingestion. Lactulose, a larger sugar molecule, should remain largely unabsorbed if the intestinal barrier is intact; however, in cases of increased permeability, more lactulose will be absorbed and excreted in urine.
- Cyrex Array #2, a blood test, measures reactivity to various food antigens and zonulin levels, providing a broader assessment of gut immunity and barrier function.
It’s crucial to understand that intestinal permeability is not a standalone diagnosis; it’s often a consequence of underlying factors like inflammation, dysbiosis, or dietary triggers. Addressing these root causes is essential for restoring gut barrier integrity. Focusing solely on “sealing” the gut without addressing the underlying issues may provide temporary relief but won’t prevent recurrence of permeability.
It is important to reiterate that this information is for educational purposes only and should not be considered medical advice. Always consult with a qualified healthcare professional for diagnosis and treatment of any health condition.