Chronic bloating affects millions worldwide, significantly impacting quality of life. It’s often dismissed as a minor inconvenience, but for those who experience it consistently, it can be debilitating – leading to discomfort, social anxiety, and even psychological distress. The complexity of the digestive system means pinpointing the exact cause is frequently challenging, making effective management elusive. Traditional approaches often focus on dietary elimination, which can be restrictive and doesn’t always address the underlying mechanisms driving the bloating. Increasingly, a more nuanced understanding of the gut-brain connection is leading to innovative therapies like gut biofeedback, offering potential for long-term relief beyond symptom management.
The frustration with chronic bloating stems from its multifaceted nature. It isn’t simply about ‘too much gas’. Factors ranging from food sensitivities and imbalances in gut microbiome https://vitagastro.com/the-role-of-gut-microbiome-in-food-sensitivity/ to stress levels and even altered motility can all contribute. Many individuals find themselves caught in a cycle of restrictive diets, only to experience bloating return as soon as they reintroduce foods. This highlights the need for strategies that go beyond dietary changes and address the physiological processes within the digestive system itself – specifically, how the gut and brain communicate. Gut biofeedback offers a promising avenue towards restoring this communication and improving digestive function, ultimately reducing chronic bloating.
Understanding the Gut-Brain Axis and Dysmotility
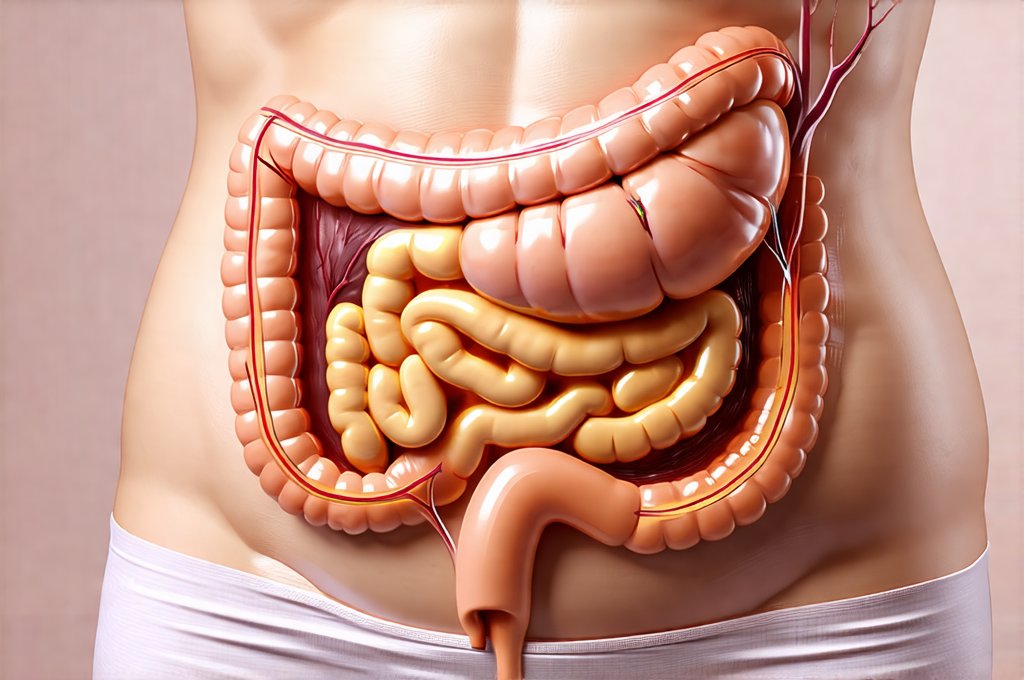
The gut isn’t an isolated organ; it’s intimately connected to the brain via what is known as the gut-brain axis. This bidirectional communication highway involves neural pathways (like the vagus nerve), hormonal signals, and importantly, the microbiome. The health of our gut profoundly influences our mental state, and conversely, our emotional state significantly impacts our digestive function. Stress, anxiety, and even mild psychological distress can disrupt normal digestive processes, leading to symptoms like bloating, altered bowel habits, and abdominal pain.
A key component often implicated in chronic bloating is dysmotility – an irregularity in the movement of food through the digestive tract. This can manifest as either accelerated or slowed motility. Slowed motility allows more time for fermentation within the gut, creating excessive gas production and causing bloating. Conversely, rapid transit can prevent proper nutrient absorption and lead to osmotic imbalances that also contribute to discomfort. Dysmotility isn’t always a structural issue; it’s often a functional problem related to the nervous system’s control over digestive muscles. This is where biofeedback comes into play, as it offers a non-invasive way to retrain these muscle movements.
Biofeedback provides real-time feedback on physiological processes – in this case, the contractions of intestinal muscles. Through specialized sensors and visual or auditory cues, individuals can learn to consciously influence their digestive function. This isn’t about directly controlling the gut; it’s about becoming aware of how your body is functioning and learning techniques to modify muscle activity through focused attention and relaxation. The goal is to restore a more balanced and coordinated pattern of intestinal motility, reducing fermentation and alleviating bloating symptoms.
How Gut Biofeedback Works: A Step-by-Step Overview
Gut biofeedback sessions typically involve several stages, tailored to the individual’s needs but generally following this framework:
- Initial Assessment: This involves a thorough evaluation of your medical history, dietary habits, and symptom presentation. It may also include testing for food sensitivities or imbalances in gut health https://vitagastro.com/the-role-of-gut-health-in-food-reactions/. The primary focus is understanding your specific bloating triggers and patterns.
- Sensor Placement: Small, external sensors are attached to the abdomen to detect intestinal muscle activity. These sensors don’t penetrate the skin; they simply measure the electrical signals produced by muscle contractions.
- Real-Time Feedback: As you perform simple exercises – often involving breathing techniques or guided imagery – your muscle activity is displayed on a screen or conveyed through auditory cues. This allows you to see (or hear) how your digestive muscles are responding.
- Muscle Training: Guided by the biofeedback therapist, you learn techniques to consciously modify your muscle contractions. This might involve practicing coordinated abdominal breathing – inhaling deeply to relax the abdomen and exhaling to gently stimulate intestinal movement.
- Progressive Practice: Sessions gradually progress from guided exercises to more independent practice, with the goal of integrating these skills into daily life. The aim is for you to be able to manage your symptoms independently between sessions.
The process emphasizes mindful awareness and self-regulation. It’s not about forcing muscles to contract; it’s about learning to influence them through gentle techniques and focused attention. Regular practice leads to improved neuromuscular control, reducing dysmotility and promoting healthier digestive function. The number of sessions varies depending on individual needs and progress, but typically ranges from 6–12 sessions.
Identifying Underlying Patterns & Personalized Approaches
One of the key benefits of gut biofeedback is its ability to identify individual patterns of dysmotility. Bloating isn’t a one-size-fits-all condition; different individuals experience it in unique ways. Biofeedback allows therapists to pinpoint specific areas of dysfunction and tailor treatment accordingly. For example:
- Someone with slowed motility might benefit from techniques designed to stimulate intestinal movement, such as rhythmic abdominal breathing synchronized with visualization exercises.
- An individual experiencing alternating constipation and diarrhea (suggesting erratic motility) might require a more comprehensive approach focused on regulating overall gut function.
- Those whose bloating is strongly linked to stress may need additional support in managing anxiety and incorporating relaxation techniques into their daily routine.
This personalized approach distinguishes biofeedback from generic dietary interventions. It addresses the root cause of the dysmotility, rather than simply eliminating potential triggers without understanding why they’re causing problems. Furthermore, biofeedback can help identify which foods are truly problematic by observing how your gut responds to specific meals during sessions. This is a much more objective way to assess food sensitivities than relying solely on elimination diets. Understanding fiber https://vitagastro.com/the-role-of-fiber-in-managing-bloating/ can also play an important role in this process.
Integrating Biofeedback with Holistic Wellness Strategies
Gut biofeedback isn’t intended as an isolated treatment; it’s most effective when integrated into a broader holistic wellness plan. While it addresses the physiological aspects of dysmotility, other factors play crucial roles in managing chronic bloating. These include:
- Dietary Modifications: Although restrictive diets aren’t always necessary, making mindful food choices and identifying personal trigger foods remains important. Biofeedback can help refine this process.
- Stress Management: Incorporating stress-reducing techniques like mindfulness meditation, yoga, or deep breathing exercises is essential for supporting gut health.
- Regular Exercise: Physical activity promotes healthy digestion and reduces stress levels. Even moderate exercise can have a significant impact on bloating symptoms.
- Hydration: Adequate hydration is crucial for maintaining regular bowel movements and preventing constipation.
- Microbiome Support: While not always necessary, exploring ways to support a diverse gut microbiome (through prebiotics and probiotics) may also be beneficial, in conjunction with biofeedback therapy.
Importantly, it’s vital to work with qualified healthcare professionals – including gastroenterologists, registered dietitians, and certified biofeedback therapists – to develop a comprehensive treatment plan tailored to your individual needs. Biofeedback isn’t a quick fix; it requires commitment and consistent practice, but the potential for long-term relief from chronic bloating makes it a valuable tool for improving digestive health and overall well-being. Considering acupuncture https://vitagastro.com/the-role-of-acupuncture-in-managing-bloating/ may also offer complementary benefits. Additionally, understanding intestinal pressure https://vitagastro.com/the-role-of-intestinal-pressure-in-chronic-heartburn/ can help you better understand your symptoms and work with your healthcare provider to develop the most effective treatment plan. Finally, incorporating a banana https://vitagastro.com/the-role-of-banana-in-managing-reflux-naturally/ into your diet could also offer some relief.