Chronic bloating is an incredibly frustrating symptom experienced by millions, often leading to discomfort, social anxiety, and a significant impact on quality of life. It’s frequently dismissed as “just gas” or attributed to dietary indiscretions, but for those who experience it persistently, the underlying causes can be complex and multifaceted. While many factors contribute – ranging from food sensitivities to stress levels – one often overlooked aspect is colon transit time, the speed at which waste moves through the large intestine. Understanding this process, and how disruptions to it might play a role in chronic bloating, can be a crucial step towards finding effective relief and improving digestive health. It’s important to remember that everyone’s digestive system is unique; what’s “normal” for one person may not be normal for another.
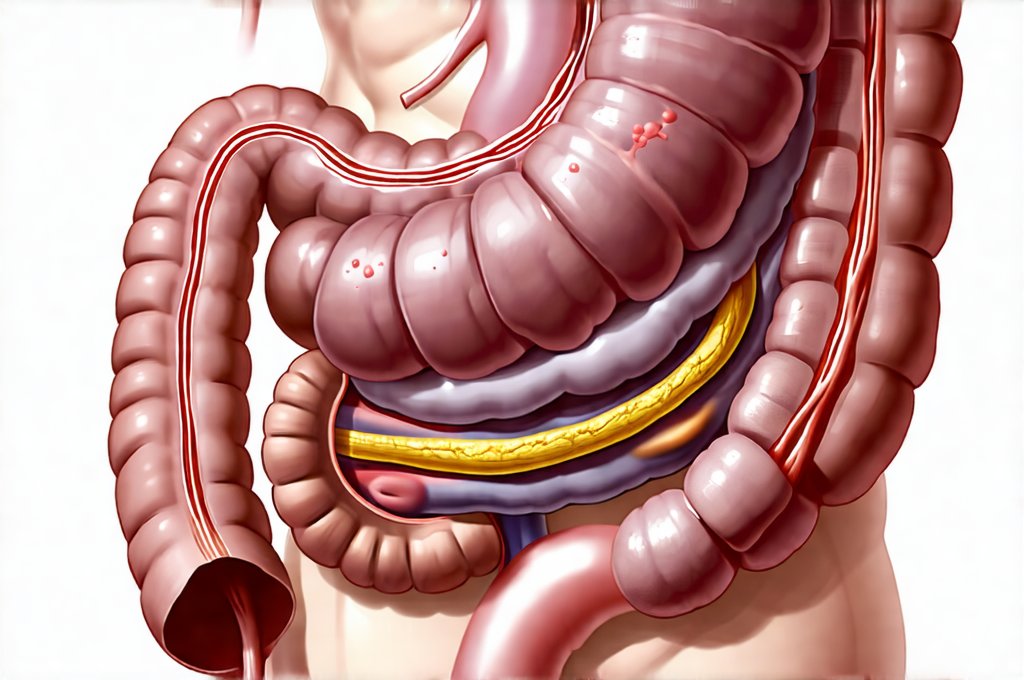
The large intestine, or colon, isn’t simply a passive holding tank for waste. It’s a dynamic environment where crucial processes like water absorption and bacterial fermentation take place. These processes are heavily influenced by the speed at which contents move through it – that is, colon transit time. Too rapid a transit can lead to insufficient nutrient absorption and potentially diarrhea, while too slow a transit can result in constipation, increased gas production due to prolonged bacterial activity, and ultimately, bloating. This delicate balance is easily disrupted by a variety of factors including diet, hydration levels, stress, physical activity, medication, and underlying medical conditions. Identifying whether your colon transit time is contributing to your bloating requires a nuanced understanding of the digestive process and potentially some investigation with healthcare professionals. Understanding how intestinal pressure affects chronic issues can be beneficial as well.
Colon Transit Time: The Basics & Its Impact on Bloating
Colon transit time refers to the amount of time it takes for food waste to travel from the cecum (the beginning of the large intestine) to the rectum. A “normal” range is typically considered between 24 and 72 hours, although this can vary significantly depending on individual factors. However, chronic bloating often arises when transit time deviates considerably from this range – either too fast or too slow. When waste lingers in the colon for an extended period (slow transit), it creates a breeding ground for bacteria. As these bacteria ferment undigested food particles, they produce excessive gas as a byproduct, leading to abdominal distension and discomfort. Conversely, rapid transit can result in insufficient breakdown of carbohydrates, also resulting in fermentation higher up in the digestive tract and subsequent bloating.
The composition of your gut microbiome plays a significant role too. An imbalance in gut bacteria (dysbiosis) – where harmful bacteria outnumber beneficial ones – can exacerbate both slow and fast transit issues. Harmful bacteria tend to produce more gas, while a lack of diversity can impair the colon’s ability to efficiently process food. Furthermore, a slowed transit time allows for increased bacterial overgrowth, amplifying these effects. It is also worth noting that individuals with conditions like Irritable Bowel Syndrome (IBS) often experience altered colonic motility – the muscle contractions that move waste through the colon – which can contribute to irregular transit times and associated bloating. Looking into acupuncture as a potential aid is something to consider.
Ultimately, bloating isn’t simply about how much gas is produced; it’s also about how effectively the digestive system handles it. A healthy colon efficiently moves gas along, minimizing discomfort. But when transit time is disrupted, that gas accumulates, leading to painful bloating and a feeling of fullness even after minimal food intake. Identifying your personal “normal” transit time – and recognizing deviations from it – can be a valuable tool in understanding the root cause of your bloating.
Dietary Strategies for Optimizing Colon Transit Time
Adjusting your diet is often the first line of defense when addressing colon transit time issues. A key component is increasing dietary fiber intake, but it’s crucial to do so gradually and choose the right types of fiber. – Soluble fiber (found in oats, beans, apples) absorbs water and forms a gel-like substance, softening stool and promoting regularity. – Insoluble fiber (found in whole grains, vegetables) adds bulk to stool and helps move waste through the digestive tract more quickly. A sudden increase in fiber can actually worsen bloating, so it’s best to add small amounts incrementally over several weeks while monitoring your body’s response. Fiber plays a huge role in digestive health.
Beyond fiber, staying adequately hydrated is essential. Water softens stool and facilitates its movement through the colon. Aim for at least eight glasses of water per day, and even more if you are physically active or live in a hot climate. Some foods can exacerbate bloating, so identifying and reducing these trigger foods is also helpful. Common culprits include: – Highly processed foods – Artificial sweeteners – Carbonated beverages – Certain FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) – found in various fruits, vegetables, and grains. An elimination diet under the guidance of a healthcare professional can help pinpoint specific food sensitivities. Understanding FODMAPs is often crucial for identifying trigger foods.
Finally, consider incorporating probiotic-rich foods into your diet. Probiotics are beneficial bacteria that can help restore balance to your gut microbiome, improving digestive function and potentially reducing bloating. Foods like yogurt (with live cultures), kefir, sauerkraut, and kimchi are excellent sources of probiotics. Remember, dietary changes should be tailored to individual needs and tolerances; what works for one person may not work for another. The importance of hydration cannot be overstated either.
The Role of Physical Activity & Stress Management
Physical activity plays a surprisingly significant role in regulating colon transit time. Regular exercise stimulates intestinal muscle contractions (peristalsis), helping to move waste through the digestive tract more efficiently. This doesn’t necessarily mean intense workouts; even moderate activities like walking, yoga, or swimming can make a difference. Aim for at least 30 minutes of physical activity most days of the week. The key is consistency – incorporating movement into your daily routine will yield better results than sporadic bursts of exercise.
Stress and anxiety are notorious disruptors of digestive function. When you’re stressed, your body releases cortisol, a hormone that can slow down digestion and alter gut motility. This can lead to constipation, increased gas production, and bloating. Mindfulness practices, such as meditation, deep breathing exercises, or yoga, can help manage stress levels and improve digestive health. Techniques like progressive muscle relaxation can also be beneficial.
Furthermore, creating a calm and relaxed eating environment is crucial. Eating quickly while stressed can impair digestion and contribute to bloating. Take your time, chew your food thoroughly, and focus on enjoying your meal. Consider journaling about your stress levels and digestive symptoms to identify potential connections between the two. Ultimately, addressing both physical activity and stress management are vital components of a holistic approach to optimizing colon transit time and reducing chronic bloating.
Investigating Underlying Medical Conditions & Seeking Professional Guidance
While dietary and lifestyle adjustments can often alleviate bloating related to altered colon transit time, it’s important to rule out any underlying medical conditions that might be contributing factors. Several conditions can affect colonic motility and cause persistent bloating, including: – Irritable Bowel Syndrome (IBS) – Small Intestinal Bacterial Overgrowth (SIBO) – Celiac Disease – Inflammatory Bowel Disease (IBD) – Crohn’s disease or ulcerative colitis. If your bloating is severe, chronic, or accompanied by other concerning symptoms like weight loss, blood in the stool, or abdominal pain, it’s crucial to consult a healthcare professional.
A doctor can perform various tests to assess your colon transit time and identify any underlying medical issues. These may include: – Lactose Breath Test – to rule out lactose intolerance – Stool Tests – to check for infections or parasites – Colonoscopy – to examine the colon for abnormalities – Hydrogen breath tests – to detect SIBO. Once a diagnosis is made, your doctor can recommend appropriate treatment options. Digestive enzymes may also be recommended in some cases.
It’s important not to self-diagnose or attempt to treat chronic bloating without professional guidance. A healthcare provider can help you develop a personalized plan that addresses your specific needs and concerns. They may also refer you to a registered dietitian for specialized dietary advice. Remember, chronic bloating is often a symptom of an underlying issue, and addressing that root cause is the key to long-term relief. Bitter foods can also support digestive health.