Acid reflux and bloating are two incredibly common digestive complaints that often go hand-in-hand, leaving many people feeling uncomfortable and seeking answers. While seemingly distinct issues – one involving heartburn and rising stomach acid, the other a sensation of fullness and gas – their interconnectedness is significant. Understanding this relationship isn’t about self-diagnosing or replacing professional medical advice; it’s about empowering individuals to better understand their bodies and potentially identify contributing factors to improve their digestive health. Many people experience occasional bouts of both, but for others, these symptoms can become chronic, severely impacting quality of life.
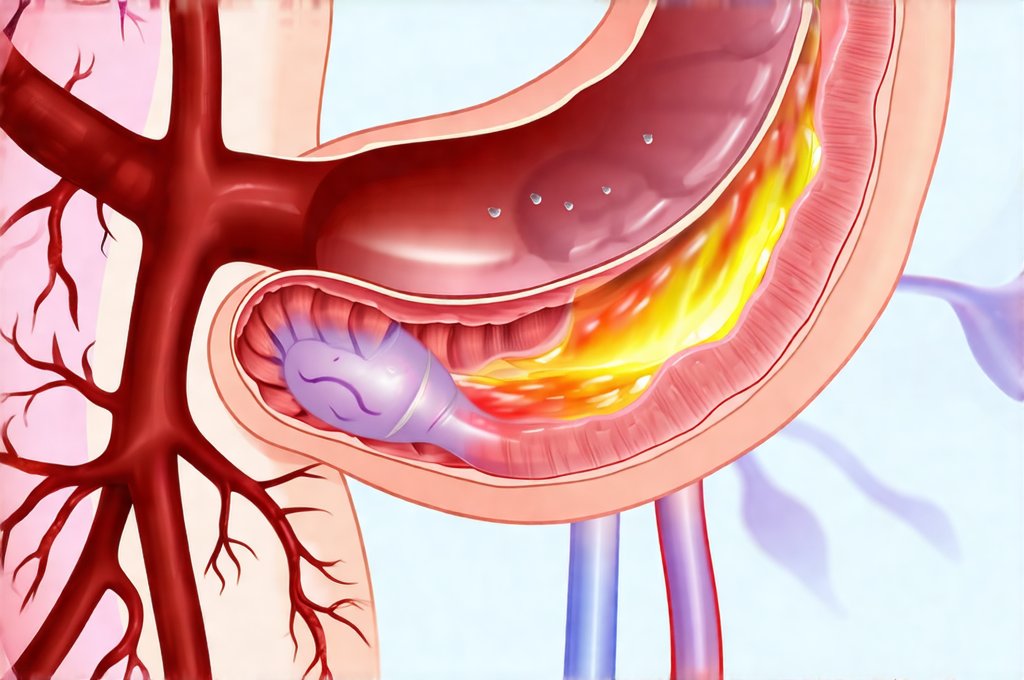
The digestive system is a complex network, and disruptions in one area frequently ripple through others. Acid reflux, formally known as gastroesophageal reflux disease (GERD), occurs when stomach acid flows back up into the esophagus, causing irritation. Bloating, on the other hand, stems from excess gas production or difficulty moving gas through the digestive tract. The connection lies in how these processes influence each other and often share underlying causes related to diet, lifestyle, and even anatomical factors. It’s essential to recognize that while they frequently occur together, they don’t always have a direct causal link; one can exist without the other, but their simultaneous presence suggests a deeper investigation into digestive health might be worthwhile. Understanding the impact of gut microbiota on overall health is also crucial for preventing these issues.
The Physiological Link Between Reflux and Bloating
The connection between acid reflux and bloating isn’t always straightforward, but several physiological mechanisms explain why they so often co-occur. One key factor is delayed gastric emptying. When the stomach takes too long to empty its contents, food remains there for longer periods, fermenting and producing more gas – leading to bloating. This delayed emptying can also increase pressure within the stomach, making reflux more likely. Furthermore, the act of swallowing air (aerophagia), often subconscious, contributes to bloating. In individuals with reflux, changes in esophageal motility—the wave-like muscle contractions that move food down—can lead to increased swallowing and therefore greater aerophagia.
Another contributing factor is the impact of acid on digestion. When stomach acid repeatedly flows into the esophagus, it can disrupt normal digestive processes further down the line. This disruption might alter the gut microbiome – the community of bacteria in your intestines – potentially leading to imbalances that increase gas production. Specifically, changes in bacterial populations can favor gas-producing strains. The vagus nerve, a crucial component of the gut-brain axis, also plays a role; chronic irritation from reflux may affect its function, contributing to both bloating and altered digestive motility. Acid reflux and anxiety often go hand in hand due to this connection.
Finally, it’s important to consider that some treatments for acid reflux can inadvertently exacerbate bloating. For example, proton pump inhibitors (PPIs), commonly prescribed medications, can alter the gut microbiome in some individuals, leading to increased gas production and discomfort. This highlights the importance of working with a healthcare provider to find the most appropriate treatment plan, balancing symptom relief with potential side effects.
Dietary Triggers and Their Impact
Diet plays a massive role in both acid reflux and bloating. Certain foods are well-known triggers for reflux – spicy foods, fatty foods, chocolate, caffeine, alcohol, and citrus fruits all relax the lower esophageal sphincter (LES), allowing stomach acid to escape. However, many of these same foods can also contribute to bloating. Fatty foods, in particular, take longer to digest, increasing gas production. Carbonated beverages introduce air into the digestive system directly, while artificial sweeteners and sugar alcohols found in diet products are poorly absorbed by the gut and ferment readily, leading to bloating and discomfort.
Beyond specific food items, eating habits themselves can significantly impact both conditions. Eating large meals quickly overwhelms the digestive system, increasing pressure on the LES and slowing down gastric emptying. This leads to more acid reflux and greater gas production. Similarly, gulping air while eating or drinking contributes directly to bloating. Food intolerances and sensitivities – such as lactose intolerance or gluten sensitivity – can also be significant drivers of both symptoms; undigested food ferments in the gut, producing gas and potentially triggering inflammation that worsens reflux. The connection between bloating and constipation can further complicate these issues.
Identifying dietary triggers often requires a process of elimination. Keeping a detailed food diary, noting what you eat and when your symptoms occur, can help pinpoint problematic foods. A healthcare professional or registered dietitian can assist with this process, providing guidance on eliminating potential culprits and reintroducing them gradually to assess tolerance levels. Remember, everyone is different; there isn’t a one-size-fits-all dietary solution.
Identifying Underlying Conditions
While diet and lifestyle are often major contributors, persistent acid reflux and bloating could signal underlying medical conditions requiring diagnosis and treatment. Irritable Bowel Syndrome (IBS) is a common functional gastrointestinal disorder characterized by abdominal pain, bloating, gas, diarrhea, and constipation. It frequently overlaps with GERD symptoms, making it crucial to differentiate the two or identify if both are present simultaneously. Another possibility is Small Intestinal Bacterial Overgrowth (SIBO), where excessive bacteria in the small intestine ferment undigested carbohydrates, leading to bloating, gas, and malabsorption—which can also worsen reflux by altering gut motility.
Gastroparesis, a condition where the stomach empties too slowly, is another potential underlying cause. It’s often associated with diabetes but can occur independently. Delayed gastric emptying contributes significantly to both acid reflux and bloating, creating a vicious cycle of discomfort. Less commonly, conditions like celiac disease (an autoimmune reaction to gluten) or pancreatic insufficiency (reduced enzyme production by the pancreas) can also manifest as persistent digestive issues resembling reflux and bloating. Gut pain and additives should be considered if symptoms persist.
It’s vital to consult with a healthcare professional if symptoms are severe, frequent, or don’t respond to lifestyle modifications. Diagnostic tests – such as endoscopy, breath tests for SIBO, gastric emptying studies, and allergy/intolerance testing—can help identify underlying conditions and guide appropriate treatment strategies. Self-treating without proper diagnosis can mask serious issues and delay effective care.
Lifestyle Modifications for Relief
Beyond dietary changes, several lifestyle modifications can provide significant relief from both acid reflux and bloating. Maintaining a healthy weight is crucial, as excess weight puts pressure on the abdomen and increases the risk of reflux. Regular exercise improves digestive motility and reduces stress – both contributing factors to gut health. Stress management techniques such as yoga, meditation, or deep breathing exercises can also be incredibly beneficial, as stress often exacerbates digestive symptoms.
Elevating the head of your bed by 6-8 inches during sleep can help prevent nighttime reflux. Avoid eating within 2-3 hours of bedtime to allow sufficient time for digestion. Consider smaller, more frequent meals instead of large ones. Chewing food thoroughly aids digestion and reduces air swallowing. Finally, avoiding tight-fitting clothing can also minimize pressure on the abdomen. Acid reflux and nausea are frequently connected symptoms that may require similar lifestyle adjustments.
When to Seek Professional Help
Knowing when to seek professional help is crucial. Occasional acid reflux or bloating that responds to lifestyle changes typically doesn’t require medical attention. However, if symptoms are persistent, severe, or accompanied by other concerning signs, it’s essential to consult a healthcare provider. These warning signs include: – Difficulty swallowing (dysphagia) – Unintentional weight loss – Chest pain – especially if accompanied by shortness of breath – Vomiting blood or having black, tarry stools – Severe abdominal pain – Persistent nausea and vomiting
A healthcare professional can accurately diagnose the underlying cause of your symptoms and recommend appropriate treatment options. These might include medications to reduce acid production (like PPIs or H2 blockers), prokinetic agents to improve gastric emptying, or therapies to manage IBS or SIBO. Remember, proactive management and seeking timely medical attention are key to improving digestive health and quality of life. Don’t hesitate to advocate for your own health and well-being. Gut microbiota and obesity can also play a role in overall digestive health, so it’s important to understand the connection.