Gastroesophageal reflux disease (GERD) is far more than just occasional heartburn. While many experience it as an uncomfortable annoyance, left unaddressed over years—even decades—untreated GERD can quietly erode quality of life and lead to a cascade of serious health complications extending well beyond the esophagus. It’s crucial to understand that what begins as infrequent acid reflux isn’t simply something you “get used to” or manage with antacids alone; it signals an underlying physiological issue requiring attention. Ignoring persistent symptoms risks progressive damage, impacting not just digestive health but potentially respiratory, dental, and even cardiovascular systems.
The insidious nature of long-term untreated GERD stems from the chronic exposure of the esophagus (and other organs) to stomach acid. This constant irritation isn’t a sudden event; it’s a gradual process that weakens tissues, alters physiological functions, and creates opportunities for secondary health problems to develop. Many individuals normalize their symptoms or attribute them to stress or diet, delaying diagnosis and treatment. The consequences can range from debilitating discomfort to life-threatening conditions, making early intervention paramount. This article will explore the long-term effects of untreated GERD, emphasizing why proactive management is essential for maintaining overall health and wellbeing.
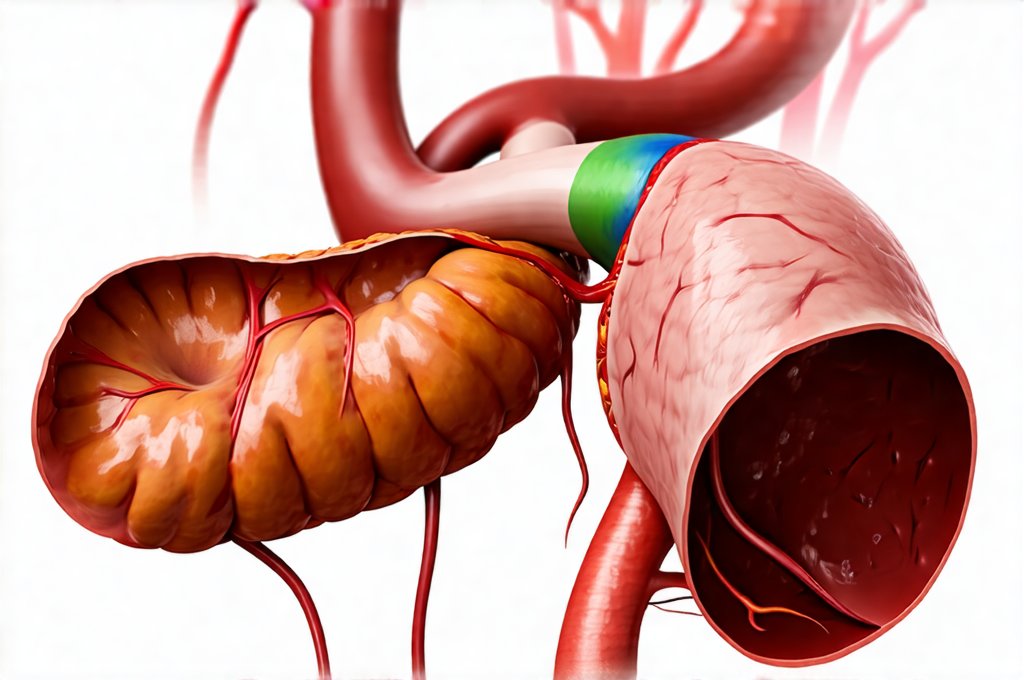
Complications Within the Digestive System
The most immediate and predictable consequences of chronic, untreated GERD are within the digestive system itself. The continuous backflow of stomach acid damages the esophageal lining, leading to several progressive conditions. – Esophagitis, inflammation of the esophagus, is often the first noticeable stage beyond occasional heartburn. Over time, this inflammation can transition into more severe problems. A key concern is Barrett’s Esophagus. This occurs when the normal cells lining the esophagus are replaced by cells similar to those found in the intestine—a metaplastic change caused by chronic acid exposure. Barrett’s Esophagus isn’t usually symptomatic itself, but it significantly increases the risk of esophageal adenocarcinoma, a relatively rare but aggressive form of cancer.
Beyond the esophagus, prolonged reflux can impact other areas of the digestive tract. The stomach itself may experience damage from repeated acid exposure—although less common than esophageal issues due to its natural defenses—leading to chronic gastritis or ulcers. More subtly, GERD can disrupt normal digestive processes higher up in the system. – Difficulty digesting food properly – Nutrient absorption problems – Changes in gut microbiome composition are all potential consequences of a chronically irritated and dysfunctional digestive tract. The impact on nutrient absorption is especially concerning as it can lead to deficiencies over time, further exacerbating health issues.
The development of strictures, or narrowings of the esophagus, is another long-term complication. These occur when scar tissue forms from chronic inflammation, making swallowing difficult. In severe cases, this necessitates medical intervention to widen the esophagus. Furthermore, untreated GERD can contribute to hiatal hernias—where a portion of the stomach protrudes through the diaphragm—worsening reflux symptoms and creating a vicious cycle of damage. It’s important to remember that these complications are not inevitable; consistent management of GERD significantly reduces their likelihood.
Esophageal Cancer & Barrett’s Esophagus: A Serious Progression
Barrett’s esophagus is arguably the most concerning long-term complication of untreated GERD, primarily because it dramatically increases the risk of esophageal adenocarcinoma. It’s estimated that individuals with Barrett’s have a 30 to 60 times higher risk than those without. This isn’t a direct transformation; rather, Barrett’s represents a precancerous condition where cellular changes create an environment more susceptible to cancerous development. – Regular endoscopic surveillance is critical for patients diagnosed with Barrett’s Esophagus. Endoscopies allow doctors to monitor the esophageal lining for dysplasia (abnormal cell growth) – a key indicator of cancer risk.
The progression from Barrett’s to adenocarcinoma isn’t automatic, and many individuals with Barrett’s never develop cancer. However, early detection through surveillance allows for interventions like endoscopic ablation or resection—procedures designed to eliminate dysplastic cells before they progress into full-blown cancer. – The importance of lifestyle modifications and medication (like proton pump inhibitors) in managing GERD and potentially slowing or even reversing some aspects of Barrett’s Esophagus cannot be overstated. While it doesn’t guarantee prevention, proactive management significantly reduces risk.
It’s crucial to understand that esophageal cancer often presents with subtle symptoms in its early stages, making it difficult to detect without regular screening. Symptoms like difficulty swallowing (dysphagia), weight loss, and chest pain may not appear until the disease is advanced. This underscores the importance of addressing GERD proactively and seeking medical attention if you experience persistent heartburn or other digestive issues.
Complications Beyond the Esophagus: The Systemic Effects
The effects of long-term untreated GERD aren’t confined to the digestive system; they can extend to other parts of the body, creating a range of health problems seemingly unrelated to stomach acid. One significant area impacted is respiratory health. – Chronic aspiration—the accidental inhalation of stomach contents into the lungs—is common in individuals with GERD. This can lead to chronic cough, asthma exacerbations, pneumonia, and even lung damage over time. The acidity irritates the delicate lung tissues, increasing susceptibility to infections and inflammation.
Another often overlooked consequence is dental erosion. Stomach acid refluxing into the mouth can erode tooth enamel, leading to increased sensitivity, cavities, and overall dental health problems. This isn’t simply a cosmetic issue; it can significantly impact quality of life and necessitate extensive dental work. – Maintaining good oral hygiene practices (brushing after meals) and discussing GERD management with your dentist are important steps in protecting your teeth.
Furthermore, there’s growing evidence linking chronic GERD to an increased risk of laryngitis, inflammation of the voice box, and even vocal cord damage. This can result in hoarseness, difficulty speaking, and changes in voice quality. While less common than some other complications, these respiratory and dental effects highlight the systemic nature of untreated GERD and its far-reaching consequences.
The Potential Cardiovascular Link & Emerging Research
While research is ongoing, there’s an emerging body of evidence suggesting a potential link between chronic GERD and cardiovascular health. This connection isn’t fully understood, but several theories exist. – One hypothesis centers on the inflammatory response triggered by GERD. Chronic inflammation is now recognized as a key contributor to heart disease, and the persistent irritation caused by acid reflux could contribute to systemic inflammation.
Another potential mechanism involves the impact of GERD on blood pressure regulation. Some studies suggest that chronic reflux may disrupt autonomic nervous system function, leading to fluctuations in blood pressure and potentially increasing cardiovascular risk. – It’s important to note this is an area of active research, and more definitive studies are needed to establish a clear causal relationship. However, given the prevalence of both GERD and heart disease, the potential link warrants attention.
Finally, some medications used to treat GERD—particularly proton pump inhibitors (PPIs)—have been subject to scrutiny regarding their long-term cardiovascular effects. While generally considered safe, some studies have raised concerns about potential nutrient deficiencies (like magnesium) associated with PPI use, which could indirectly impact heart health. – Discussing the risks and benefits of any medication with your doctor is crucial, especially when considering long term side effects of treatment options. The key takeaway here isn’t to avoid GERD treatment; it’s to manage the condition effectively while minimizing potential side effects through informed decision-making and regular medical monitoring.
It is essential to consult with a healthcare professional for diagnosis and treatment of GERD or any related health concerns. This information is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Meal timing can also impact GERD symptoms. Finally, if you’re struggling with gut instability, seek professional help.