Brain fog – that frustrating mental state characterized by difficulty concentrating, memory lapses, and an overall feeling of sluggishness – is becoming increasingly common in modern life. Many attribute it to stress, lack of sleep, or simply being overwhelmed. However, emerging research points to a surprising and often overlooked connection: the gut. For years, the digestive system was seen as largely separate from the brain, but we now understand they are intricately linked via what’s known as the gut-brain axis. This bidirectional communication highway means that what happens in your gut can profoundly impact your cognitive function, and vice versa. Ignoring gut health when addressing brain fog is akin to treating a headache without acknowledging the underlying cause.
Digestive gas, often dismissed as an unpleasant but harmless side effect of eating, can be a significant indicator of imbalances within this crucial ecosystem. While occasional gas is normal, excessive or persistent bloating, flatulence, and abdominal discomfort can signal deeper issues impacting gut health – and consequently, brain function. This isn’t about blaming your burps for your brain fog; it’s about recognizing that these seemingly disparate symptoms may be connected pieces of a larger puzzle. The composition of our gut microbiome, the efficiency of our digestion, and even food reactions all play a role in this complex interplay. Understanding the mechanisms at work can empower you to address both digestive discomfort and cognitive cloudiness simultaneously.
The Gut-Brain Axis: A Two-Way Street
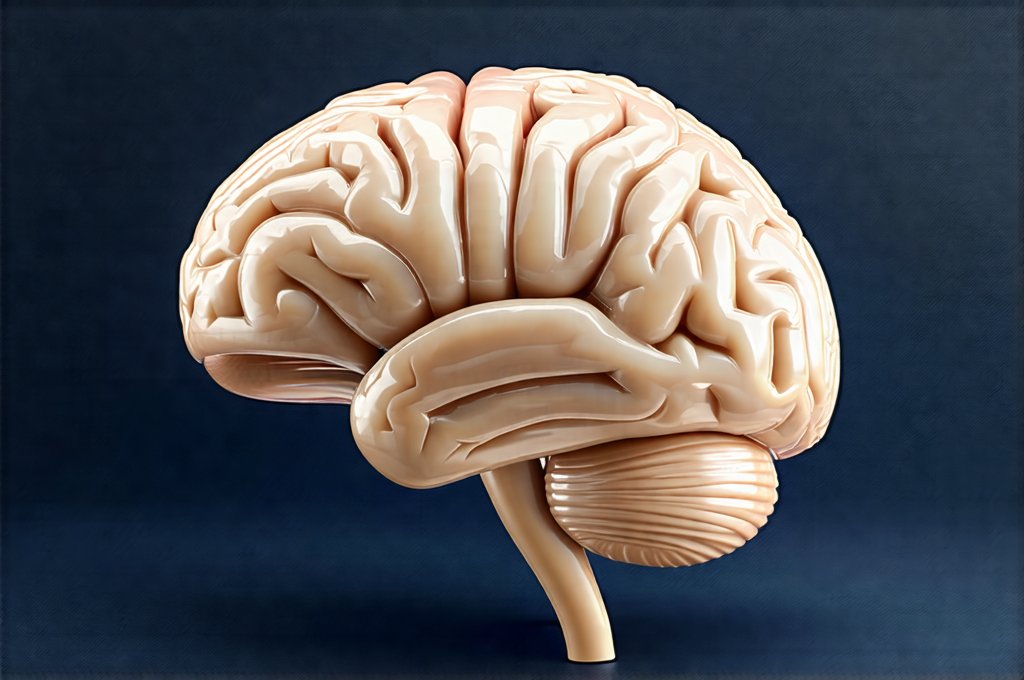
The gut-brain axis isn’t simply an anatomical connection; it’s a sophisticated communication network involving neurological, immunological, and biochemical pathways. Millions of neurons reside in the enteric nervous system – often called the “second brain” – which lines our digestive tract. This network communicates directly with the central nervous system via the vagus nerve, allowing for rapid transmission of signals between gut and brain. When the gut is inflamed or imbalanced, these signals can contribute to neuroinflammation and impaired cognitive function. Imagine a constantly buzzing phone line; it’s difficult to hear clearly when there’s constant noise. Similarly, chronic inflammation in the gut sends continuous signals that can overwhelm and disrupt brain activity.
The microbiome – the trillions of bacteria, fungi, viruses, and other microorganisms living in our digestive tract – is central to this communication. These microbes aren’t just passive bystanders; they actively produce neurotransmitters like serotonin (the “happy hormone”), dopamine, and GABA which influence mood, cognition, and overall brain health. A diverse and balanced microbiome supports optimal neurotransmitter production and reduces inflammation. Conversely, an imbalance in gut bacteria – known as dysbiosis – can lead to decreased neurotransmitter synthesis, increased inflammation, and ultimately, contribute to brain fog. Anxiety issues can also play a role in this disruption.
Furthermore, the gut is a major player in our immune system. Approximately 70-80% of our immune cells reside in the gut, constantly monitoring the microbiome and responding to potential threats. When the gut barrier becomes compromised – often referred to as “leaky gut” – undigested food particles, toxins, and bacteria can leak into the bloodstream, triggering an immune response that leads to systemic inflammation. This chronic inflammation is a well-established risk factor for cognitive decline and brain fog.
How Digestive Gas Signals Gut Imbalance
Excessive gas isn’t just embarrassing; it’s often a sign that something is amiss in your digestive system. Several factors can contribute to increased gas production, each potentially impacting the gut-brain axis. One common culprit is Small Intestinal Bacterial Overgrowth (SIBO), where an excessive number of bacteria reside in the small intestine – a place where they shouldn’t be so abundant. These bacteria ferment undigested carbohydrates, producing hydrogen, methane, and carbon dioxide gases as byproducts. This fermentation process can also damage the gut lining, contributing to leaky gut syndrome and subsequent inflammation.
Food sensitivities or intolerances are another frequent cause of digestive gas. Lactose intolerance (difficulty digesting milk sugar) and gluten sensitivity (reactivity to wheat proteins) are well-known examples, but many individuals react to other foods without realizing it. When the body struggles to digest certain foods, bacteria in the gut ferment them, leading to increased gas production and potential inflammation. Identifying and eliminating trigger foods – often through an elimination diet – can significantly reduce both digestive symptoms and cognitive impairment. Gut pain related to food additives may also be a contributing factor.
Finally, insufficient digestive enzymes can hinder proper food breakdown. Enzymes are essential for breaking down carbohydrates, proteins, and fats into absorbable components. Without adequate enzyme production (which can be due to factors like aging or pancreatic insufficiency), undigested food reaches the colon where bacteria ferment it, resulting in gas and bloating. Supplementing with digestive enzymes may help restore proper digestion and reduce gut-related symptoms.
Addressing the Link: Strategies for Improvement
Improving brain fog related to digestive gas requires a holistic approach focusing on restoring gut health and optimizing the gut-brain axis. It’s not about quick fixes; it’s about building long-term habits that support a healthy microbiome and efficient digestion. One cornerstone of this strategy is dietary modification. Focusing on a whole-foods diet rich in fiber, fruits, vegetables, and fermented foods (like yogurt, kefir, sauerkraut, kimchi) provides fuel for beneficial gut bacteria and promotes diversity within the microbiome.
Reducing inflammatory foods – such as processed foods, sugary drinks, excessive alcohol, and refined carbohydrates – is equally important. These foods can disrupt the microbiome, increase inflammation, and exacerbate digestive symptoms. Consider exploring an elimination diet under the guidance of a healthcare professional to identify potential food sensitivities. This involves removing common trigger foods for a period of time and then gradually reintroducing them to observe any reactions. Reflux positioning can also impact digestive health.
Beyond diet, stress management is crucial. Chronic stress negatively impacts gut health by altering the microbiome and increasing intestinal permeability. Practices like mindfulness meditation, yoga, deep breathing exercises, and regular physical activity can help manage stress levels and promote a healthier gut-brain connection. Prioritizing sleep is also essential as sleep deprivation disrupts both gut function and cognitive performance. Aim for 7-9 hours of quality sleep each night to allow your body to repair and restore itself.
It’s important to remember that the link between brain fog and digestive gas is complex and individualized. What works for one person may not work for another. Seeking guidance from a qualified healthcare professional – such as a gastroenterologist, functional medicine practitioner, or registered dietitian – can help you develop a personalized plan tailored to your specific needs and underlying imbalances. They can also rule out other potential causes of brain fog and provide appropriate support and monitoring. Digestive inflammation may be a contributing factor, as well as seafood discomfort.
GERD infections can also affect brain fog and digestive health.