Heartburn is one of those universally experienced sensations – a burning discomfort rising from your chest towards your throat. It’s often dismissed as just something you get after eating spicy food or too much pizza. But for many, heartburn isn’t an occasional annoyance; it’s a frequent and disruptive symptom that can significantly impact quality of life. What many people don’t realize is that not all heartburn is the same. While frequently attributed to Gastroesophageal Reflux Disease (GERD), a substantial number of individuals experience what’s increasingly recognized as functional heartburn – a condition with different underlying mechanisms and therefore, requiring a different approach to management. Distinguishing between these two can be crucial for effective treatment and avoiding unnecessary medication or interventions.
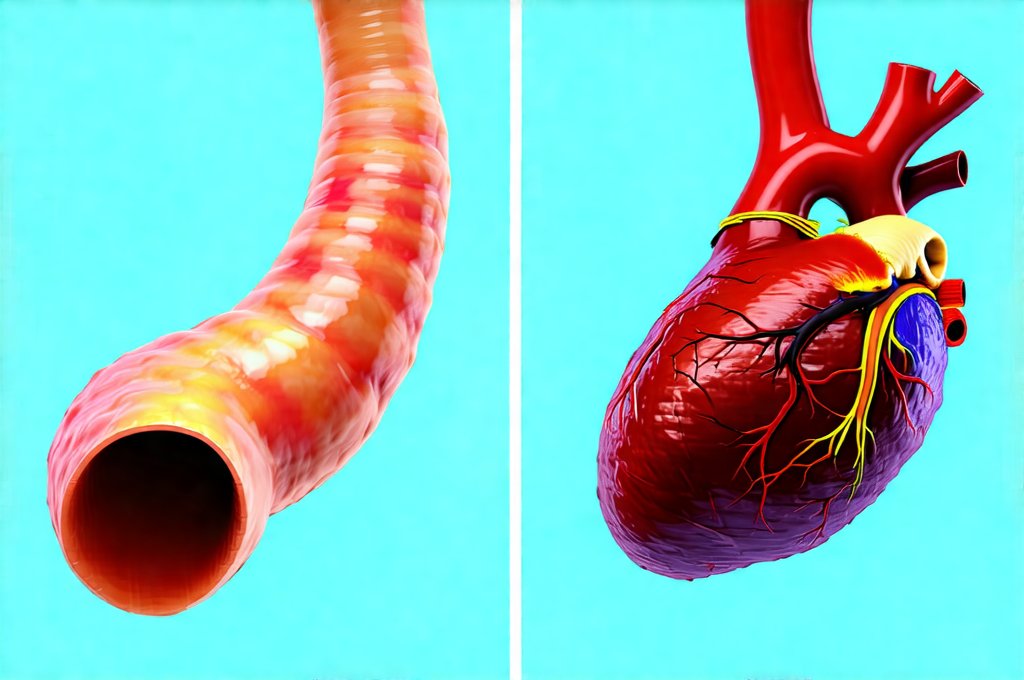
The common understanding is that heartburn stems from stomach acid flowing back up into the esophagus—the tube connecting your mouth to your stomach. This reflux irritates the esophageal lining, causing the burning sensation we associate with heartburn. However, this simple explanation doesn’t account for everyone experiencing the symptom. Functional heartburn, also known as non-erosive reflux disease (NERD), presents a more complex picture where acid reflux may not be the primary driver of the discomfort. Instead, it’s thought to involve increased sensitivity of the esophagus itself – meaning even normal amounts of stomach acid can trigger pain and discomfort. This difference is paramount in understanding how best to address the issue, as treatments focused on reducing acid production might prove ineffective for those with functional heartburn.
Understanding GERD: Acid Reflux and Esophageal Damage
Gastroesophageal Reflux Disease (GERD) isn’t simply occasional heartburn; it’s a chronic digestive disease where stomach acid frequently flows back into the esophagus. This persistent reflux can cause inflammation, damage the esophageal lining, and lead to more severe complications over time. The hallmark of GERD is often erosive esophagitis, meaning visible damage to the esophagus that can be detected during an endoscopy – a procedure involving a small camera inserted down the throat.
The underlying causes of GERD are multifaceted. Some factors contribute directly to reflux, such as:
– A weakened lower esophageal sphincter (LES), the muscle at the end of the esophagus that prevents stomach acid from flowing back up.
– Hiatal hernia, where part of the stomach protrudes through an opening in the diaphragm.
– Increased abdominal pressure from obesity or pregnancy.
Other factors can exacerbate GERD symptoms:
– Certain foods and beverages (spicy foods, fatty foods, caffeine, alcohol).
– Smoking.
– Lying down shortly after eating.
– Medications that relax the LES.
Diagnosis of GERD often involves a combination of symptom evaluation, response to proton pump inhibitor (PPI) therapy (medications that reduce stomach acid production), and potentially endoscopic examination to assess for esophageal damage. Treatment typically focuses on lifestyle modifications, medication to control acid production, or in severe cases, surgical intervention to strengthen the LES. It’s important to note that GERD is a demonstrable physiological condition with identifiable physical changes in the esophagus. Understanding the difference between allergy and sensitivity can also help understand how your body reacts to food.
Functional Heartburn: Heightened Sensitivity and Visceral Hypersensitivity
Functional heartburn differs significantly from GERD, even though the primary symptom – heartburn – is shared. In functional heartburn, acid reflux may be present, but it’s not frequent enough or severe enough to cause esophageal damage. More importantly, the perception of burning is disproportionate to the amount of acid actually reaching the esophagus. This suggests that the problem isn’t necessarily too much acid, but rather a heightened sensitivity to normal amounts of acid – a phenomenon called visceral hypersensitivity.
The exact causes of functional heartburn are still being researched, but it’s believed to be linked to:
– Altered nerve function in the esophagus.
– Increased sensitivity of pain receptors in the esophageal lining.
– Psychological factors like stress and anxiety, which can amplify pain perception.
– Brain-gut interaction issues – how well the brain and digestive system communicate.
Diagnosing functional heartburn often involves ruling out GERD first. This typically includes a trial period on PPI medication to see if symptoms improve. If PPIs don’t provide relief, and an endoscopy reveals no evidence of esophageal damage, functional heartburn becomes a strong possibility. Unlike GERD treatment which aims to reduce acid, managing functional heartburn focuses more on modulating pain perception, addressing psychological factors, and potentially using therapies that desensitize the esophagus. This condition is characterized by symptom presence without demonstrable organic disease. In some cases the connection between GERD and other symptoms like hiccups may be present, but not causative.
Diagnosing the Difference: What Tests Can Help?
Pinpointing whether you have GERD or functional heartburn isn’t always straightforward, as symptoms can overlap. A thorough evaluation by a healthcare professional is crucial. Here are some tests that might be used to differentiate between the two conditions:
- Endoscopy: As mentioned earlier, endoscopy allows for direct visualization of the esophagus and stomach, looking for signs of inflammation or damage (erosive esophagitis). A normal endoscopy strongly suggests functional heartburn rather than GERD.
- Ambulatory Reflux Monitoring: This test measures the amount of acid in the esophagus over a 24-hour period. It can help determine if reflux is occurring, and how often. However, even with significant reflux, symptoms might not correlate with acid exposure in functional heartburn, indicating hypersensitivity. There are various types of monitoring available, including impedance-pH monitoring which detects both acidic and non-acidic reflux.
- Esophageal Manometry: This test measures the pressure and coordination of muscle contractions in the esophagus. It can help identify problems with the LES or esophageal motility (how food moves down the esophagus). Abnormalities here might point toward GERD, while normal results are more consistent with functional heartburn.
It’s important to remember that tests aren’t always conclusive. A healthcare provider will consider your symptoms, medical history, and test results collectively to arrive at an accurate diagnosis. A comprehensive approach is key – relying solely on one test can be misleading. If you experience nausea alongside heartburn, it could indicate the connection between GERD and other digestive issues.
Treatment Approaches: Tailoring Therapy to the Condition
The treatment for GERD and functional heartburn differ significantly due to their distinct underlying mechanisms. For GERD, treatments typically include:
1. Lifestyle modifications: Elevating the head of your bed, avoiding trigger foods, losing weight if necessary, and quitting smoking.
2. Medications: Antacids to neutralize stomach acid, H2 blockers to reduce acid production, and PPIs to significantly suppress acid secretion.
3. Surgery: In severe cases, procedures like fundoplication can strengthen the LES.
For functional heartburn, a different approach is needed. Since acid isn’t usually the primary problem, simply reducing acid often provides little relief. Treatment strategies focus on:
– Pain management techniques: Including therapies to desensitize the esophagus and reduce visceral hypersensitivity.
– Psychological interventions: Addressing stress, anxiety, and depression, which can exacerbate symptoms. Cognitive Behavioral Therapy (CBT) has shown promise in managing functional heartburn.
– Dietary adjustments: Identifying and avoiding foods that trigger your specific discomfort, even if they aren’t typically associated with GERD.
– Medications: Low doses of antidepressants or neuromodulators may be used to help modulate pain perception.
The goal is not necessarily to eliminate acid reflux altogether (which might not even be present), but rather to manage the heightened sensitivity that causes discomfort. A multidisciplinary approach, involving a gastroenterologist, psychologist, and potentially a dietitian, can be particularly effective. Understanding the difference between allergy and sensitivity may also help identify food triggers.
Managing Symptoms Long-Term: Lifestyle and Prevention
Regardless of whether you have GERD or functional heartburn, certain lifestyle changes can help manage symptoms and improve quality of life. These include maintaining a healthy weight, avoiding trigger foods (identifying these is individualized), eating smaller more frequent meals, not lying down immediately after eating, elevating the head of your bed, and quitting smoking. For those with GERD, consistent medication adherence as prescribed by their doctor is vital to prevent esophageal damage.
For individuals with functional heartburn, ongoing stress management techniques like mindfulness, yoga, or meditation can be beneficial. Learning to identify and cope with triggers – both physical and emotional – is also crucial. It’s important to remember that functional heartburn isn’t “all in your head” – it’s a real condition with a physiological basis, but psychological factors can play a significant role in symptom perception. If throat clearing accompanies these symptoms, the connection between GERD should be considered. Regular communication with your healthcare team is essential for long-term management and adapting your treatment plan as needed. Ultimately, understanding the difference between GERD and functional heartburn allows for targeted and effective intervention, leading to better health outcomes and improved well-being. If gut pain accompanies these symptoms it could be the link between gut pain and food additives.