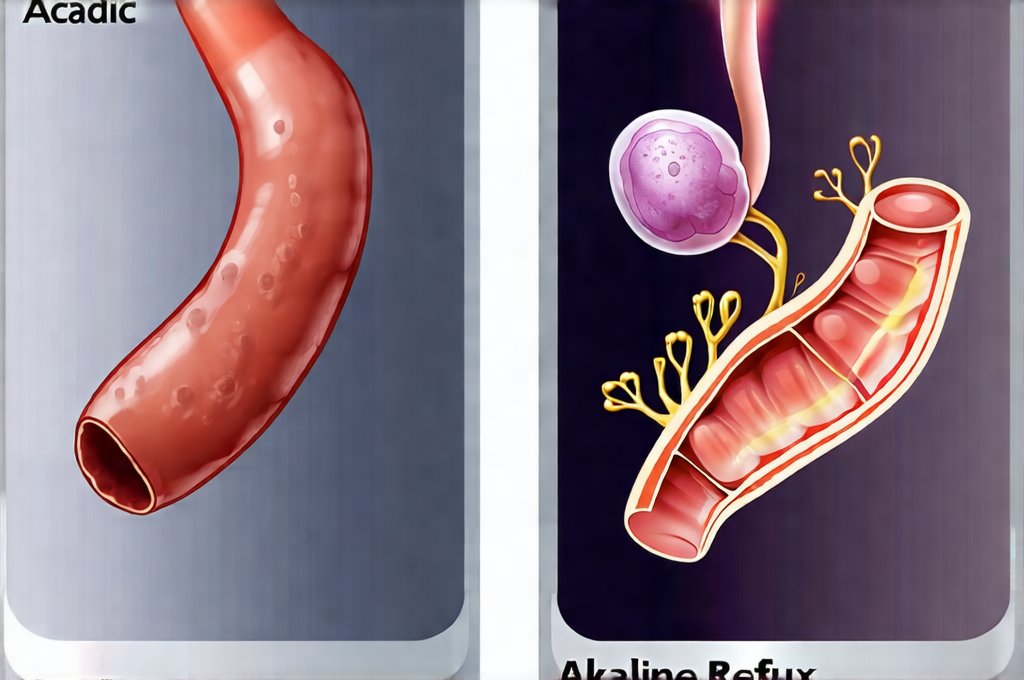
Acid reflux and alkaline reflux are both conditions arising from disruptions in the digestive system’s natural processes, frequently manifesting as heartburn or indigestion. However, despite sharing some overlapping symptoms, they stem from fundamentally different causes and require distinct understandings for effective management. Acid reflux, the more commonly recognized condition, involves stomach acid flowing back up into the esophagus. Alkaline reflux, less discussed but increasingly acknowledged, is its counterpart – a backward flow of duodenal contents, which are typically alkaline or neutral, into the stomach and sometimes even further up the digestive tract. Recognizing these differences isn’t about replacing one diagnosis with another; it’s about achieving more precise understanding for better symptom relief and potentially preventing long-term complications.
Many people assume that heartburn automatically equates to excessive acid, leading them to self-treat with antacids. While this can be helpful in some cases of acid reflux, it may actually worsen alkaline reflux symptoms. This is because antacids neutralize stomach acidity which can paradoxically encourage more duodenal content to flow upwards to balance the pH. The complexities within digestive health necessitate a nuanced approach and highlight why accurate identification of the underlying cause – acidic or alkaline reflux – is paramount for developing personalized management strategies, ideally in consultation with a healthcare professional. Understanding how [the difference between allergy and sensitivity] can play into these issues is also important.
Understanding Acid Reflux: The Classic Scenario
Acid reflux occurs when the lower esophageal sphincter (LES), a muscular ring at the bottom of the esophagus, weakens or relaxes inappropriately. This allows stomach acid to flow back up into the esophagus, irritating its sensitive lining. The sensation is often described as a burning discomfort in the chest, known as heartburn, but can also manifest as regurgitation – the feeling of sour liquid coming back up – difficulty swallowing (dysphagia), and even chronic cough or asthma-like symptoms. Factors contributing to acid reflux are diverse and include dietary choices, lifestyle habits, obesity, smoking, certain medications, and hiatal hernias where part of the stomach protrudes through the diaphragm. [The link between gut pain and additives] can also exacerbate these issues.
The typical presentation of acid reflux is relatively straightforward: a burning sensation rising from the stomach towards the throat, often triggered after meals or when lying down. However, it’s important to note that symptoms can vary greatly in intensity and frequency. Some individuals experience only mild, occasional heartburn, while others suffer from chronic, debilitating symptoms that significantly impact their quality of life. Over time, persistent acid reflux can lead to more serious complications such as esophagitis (inflammation of the esophagus), Barrett’s esophagus (a precancerous condition), and even esophageal cancer – emphasizing the importance of addressing it proactively. [Recognizing the connection between overthinking and IBS] is also important for holistic gut health.
Management of acid reflux often begins with lifestyle modifications like elevating the head of your bed, avoiding trigger foods (spicy, fatty, acidic), losing weight if overweight, and quitting smoking. Over-the-counter medications such as antacids can provide temporary relief by neutralizing stomach acid, while proton pump inhibitors (PPIs) and H2 blockers reduce acid production for longer-term management – though long-term use of these should be discussed with a doctor. The key takeaway is that acid reflux is fundamentally linked to an overabundance or improper flow of stomach acid.
Alkaline Reflux: A Less Familiar Picture
Alkaline reflux, sometimes called bile reflux, happens when the alkaline contents from the duodenum – the first part of the small intestine – flow backwards into the stomach and potentially up into the esophagus. This is often linked to problems with the pyloric valve, a muscular ring between the stomach and duodenum, or issues within the intestinal system itself. Unlike acid reflux, the symptoms aren’t necessarily caused by excess acidity; they’re frequently triggered by an imbalance of pH levels in the stomach. This can occur after gallbladder removal (cholecystectomy), where bile flow is disrupted, or due to problems with the migrating motor complex (MMC) which regulates digestive movement. [The link between food reactions and skin rashes] may also indicate underlying sensitivities.
The symptoms of alkaline reflux can be particularly challenging to distinguish from acid reflux because they often overlap. Heartburn is common, but it may feel different – less burning and more of a dull ache or discomfort. Other signs include nausea, bloating, abdominal pain, belching, and even diarrhea. A key distinguishing feature is that antacids often provide little to no relief, and can sometimes worsen the symptoms as they further disrupt stomach acidity. Some individuals with alkaline reflux report experiencing a bitter or sour taste in their mouth, though this isn’t consistent.
Diagnosing alkaline reflux requires more than just symptom evaluation. Tests like gastric drainage studies, bile acid breath tests, and endoscopic examination may be necessary to confirm the diagnosis and identify any underlying causes. Treatment focuses on restoring proper digestive function and managing symptoms. This might involve dietary changes (low-fat diets are often recommended), medications to stimulate gastric emptying or reduce bile production, and in some cases, surgical intervention to address pyloric valve dysfunction. Understanding that alkaline reflux isn’t about too much acid is critical for effective treatment. [The connection between mood and food intolerance] can play a role here as well.
Differentiating the Two: Key Indicators & Diagnostic Approaches
Pinpointing whether you’re experiencing acidic or alkaline reflux can be complex, but several indicators can help differentiate between the two. Consider these points:
- Antacid Response: If antacids consistently relieve your symptoms, it’s more likely acid reflux. If they provide little to no relief, or even worsen things, suspect alkaline reflux.
- Symptom Timing: Acid reflux often flares up after meals and when lying down. Alkaline reflux may be less tied to specific meal times and can occur more randomly throughout the day.
- Associated Symptoms: Diarrhea, bloating, and a bitter taste in the mouth are more common with alkaline reflux.
- Gallbladder History: A history of gallbladder removal significantly increases the likelihood of alkaline reflux.
Diagnostic approaches differ accordingly. For suspected acid reflux, an endoscopy can visualize the esophagus for signs of damage from acid exposure. A pH monitoring test measures acidity levels in the esophagus over a period of time (usually 24 hours). For suspected alkaline reflux, diagnostic tests are more complex. Gastric emptying studies assess how quickly food moves through your stomach and duodenum. Bile acid breath tests detect the presence of bile acids in the stomach. Endoscopy can also be used to collect samples for bile acid analysis. [The connection between salicylates and migraines] might contribute to digestive discomfort.
It’s crucial to remember that self-diagnosis is not recommended. If you’re experiencing persistent digestive symptoms, consult a healthcare professional who can properly evaluate your condition and recommend the most appropriate course of action. The distinction between acidic and alkaline reflux isn’t always clear cut, and accurate diagnosis requires specialized testing and expert medical evaluation. A personalized approach based on thorough assessment is essential for effective management. [The link between seafood and digestive discomfort] should also be considered when evaluating symptoms.
It’s important to reiterate that this information is intended for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.