Indigestion and nausea are incredibly common experiences, often dismissed as temporary discomforts stemming from something we ate. While dietary factors certainly play a role, a growing body of research points to a less obvious culprit: physical inactivity. Many individuals experience these digestive issues not because of what they’re eating, but because of how little they’re moving. Modern lifestyles are increasingly sedentary – prolonged sitting is the norm for many jobs and leisure activities – and this lack of movement has far-reaching consequences beyond weight gain or muscle loss. It disrupts fundamental physiological processes, including digestion, creating a fertile ground for symptoms like bloating, heartburn, feelings of fullness even after small meals, and ultimately, nausea. This isn’t merely about athletic performance; it’s about the basic human need for regular physical activity to maintain optimal bodily function.
The connection between movement and digestive health is deeply rooted in our evolutionary history. Our bodies evolved expecting consistent movement as part of daily life. Digestion was never designed to occur while sitting still for hours on end. The rhythmic contractions necessary for moving food through the digestive tract, the stimulation of gut motility, and even the production of digestive enzymes are all enhanced by physical activity. When we become sedentary, these processes slow down, leading to a cascade of problems that manifest as indigestion and nausea. It’s important to understand this isn’t simply a case of needing to “burn off” calories; it’s about restoring natural physiological function through movement. The implications are significant for public health, as chronic digestive issues can profoundly impact quality of life.
The Physiological Link: How Inactivity Impacts Digestion
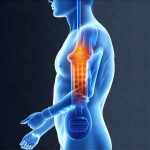
The digestive system is, at its core, a muscular process. It relies on peristalsis – wave-like muscle contractions – to move food from the esophagus down through the stomach and intestines. Physical inactivity directly weakens these muscles over time, leading to slower transit times and increased risk of constipation. This sluggish movement allows food to ferment in the gut, creating gas and bloating, which are often precursors to indigestion and nausea. Furthermore, regular exercise stimulates the vagus nerve, a crucial component of the gut-brain axis. The vagus nerve plays a vital role in regulating digestive function, promoting gastric emptying and reducing inflammation. A sedentary lifestyle diminishes vagal tone, hindering these processes.
Beyond muscle strength and nerve stimulation, physical activity also impacts hormone regulation relevant to digestion. Exercise helps regulate cortisol levels (the stress hormone), which can disrupt gut motility and contribute to indigestion when chronically elevated. It also influences the production of ghrelin and leptin – hormones that control appetite and satiety. Imbalances in these hormones, often exacerbated by inactivity, can lead to overeating or irregular eating patterns, both of which strain the digestive system. The relationship is bidirectional: a healthy gut microbiome (influenced by diet and exercise) promotes better mental health, reducing stress levels and further improving digestion.
Essentially, physical activity acts as a natural “pro-motility” agent, encouraging efficient digestion. When we sit for prolonged periods, the digestive process becomes sluggish, increasing the likelihood of discomfort and nausea. This is why even short bursts of movement throughout the day can be incredibly beneficial – it’s not about needing to run a marathon, but rather incorporating activity as an integral part of daily life.
The Role of Inflammation & Gut Microbiome
Chronic inflammation is increasingly recognized as a root cause of many health problems, and digestive issues are no exception. Physical inactivity contributes significantly to systemic low-grade inflammation. When we don’t move, our immune system becomes less efficient at resolving minor inflammatory responses. This leads to a persistent state of mild inflammation throughout the body, including the gut. A chronically inflamed gut is more susceptible to irritation and dysfunction, making individuals more prone to indigestion and nausea. Furthermore, inflammation disrupts the delicate balance of the gut microbiome – the trillions of bacteria residing in our digestive tract.
The gut microbiome plays a critical role in digestion, immunity, and even mental health. Physical activity has been shown to positively influence the diversity and composition of the gut microbiome, promoting beneficial bacterial strains that aid in digestion and reduce inflammation. Conversely, inactivity is associated with decreased microbial diversity and an increase in harmful bacteria. This imbalance can lead to increased intestinal permeability (often called “leaky gut”), allowing toxins and undigested food particles to enter the bloodstream, further exacerbating inflammation and triggering nausea.
The connection between exercise, inflammation, and gut health creates a powerful cycle: inactivity leads to inflammation, which disrupts the microbiome, leading to digestive issues, which can discourage activity, perpetuating the cycle. Breaking this cycle requires a conscious effort to incorporate regular physical movement into one’s routine. This isn’t just about symptom relief; it’s about addressing the underlying physiological factors contributing to digestive discomfort. Understanding gut inflammation is crucial for long-term health.
Addressing Indigestion & Nausea Through Movement
If you frequently experience indigestion or nausea, and suspect inactivity might be a contributing factor, here are some steps you can take:
- Start Small: Don’t feel pressured to immediately begin an intense exercise program. Begin with manageable activities like walking for 15-20 minutes each day. Gradual increases in activity are more sustainable and less likely to overwhelm your body.
- Incorporate Movement Snacks: Break up long periods of sitting with short bursts of movement throughout the day. This could include taking a quick walk during lunch breaks, doing some simple stretches at your desk, or climbing stairs instead of taking the elevator.
- Focus on Low-Impact Activities: Activities like yoga, swimming, and cycling are gentle on the digestive system while still providing significant benefits. Avoid high-intensity exercises immediately after eating.
The key is consistency. Even small amounts of regular movement can make a substantial difference in your digestive health. It’s also crucial to listen to your body and avoid pushing yourself beyond your limits. If nausea persists or worsens, consult with a healthcare professional to rule out any underlying medical conditions. Remember that addressing the root cause – in this case, physical inactivity – is more effective than simply masking symptoms. In some cases, nausea might be connected to food poisoning.
The Importance of Mindful Movement & Stress Reduction
While exercise is beneficial, it’s equally important to incorporate mindful movement practices into your routine. Activities like yoga and Tai Chi not only promote physical activity but also emphasize deep breathing and relaxation techniques. These techniques help reduce stress levels, which, as mentioned earlier, can significantly impact digestive function. Chronic stress triggers the release of cortisol, disrupting gut motility and exacerbating inflammation.
Mindful movement encourages a greater awareness of your body’s signals, allowing you to recognize early signs of indigestion or nausea and adjust your activity level accordingly. It also promotes a sense of calm and well-being, which can further improve digestive health. Furthermore, stress reduction techniques like meditation and deep breathing exercises can be used independently to manage stress levels and alleviate digestive symptoms. Recognizing the role of stress is key for holistic wellness.
Beyond Exercise: Lifestyle Factors & Holistic Approach
It’s vital to remember that physical activity is just one piece of the puzzle. A holistic approach to digestive health involves addressing other lifestyle factors that contribute to indigestion and nausea. This includes:
- Diet: Consume a balanced diet rich in fiber, fruits, vegetables, and lean protein. Avoid processed foods, sugary drinks, and excessive amounts of caffeine or alcohol.
- Hydration: Drink plenty of water throughout the day to keep your digestive system functioning optimally.
- Sleep: Aim for 7-8 hours of quality sleep each night. Sleep deprivation can disrupt hormone balance and increase stress levels, both of which impact digestion.
- Eating Habits: Eat smaller, more frequent meals rather than large, infrequent ones. Chew your food thoroughly to aid in digestion. Avoid eating late at night.
Ultimately, the connection between physical inactivity and increased episodes of indigestion and nausea highlights the importance of integrating movement into our daily lives not just for fitness, but for overall health and well-being. By understanding the physiological mechanisms involved and adopting a holistic approach that encompasses both exercise and lifestyle modifications, we can significantly improve our digestive health and reduce the frequency and severity of these common discomforts. Prioritizing physical activity is an investment in your long-term health and quality of life. Sometimes nausea is connected to hormonal changes. It’s also important to note the impact of high-fat diets on digestive health. If you suspect GERD is contributing, learn about GERD and nausea.