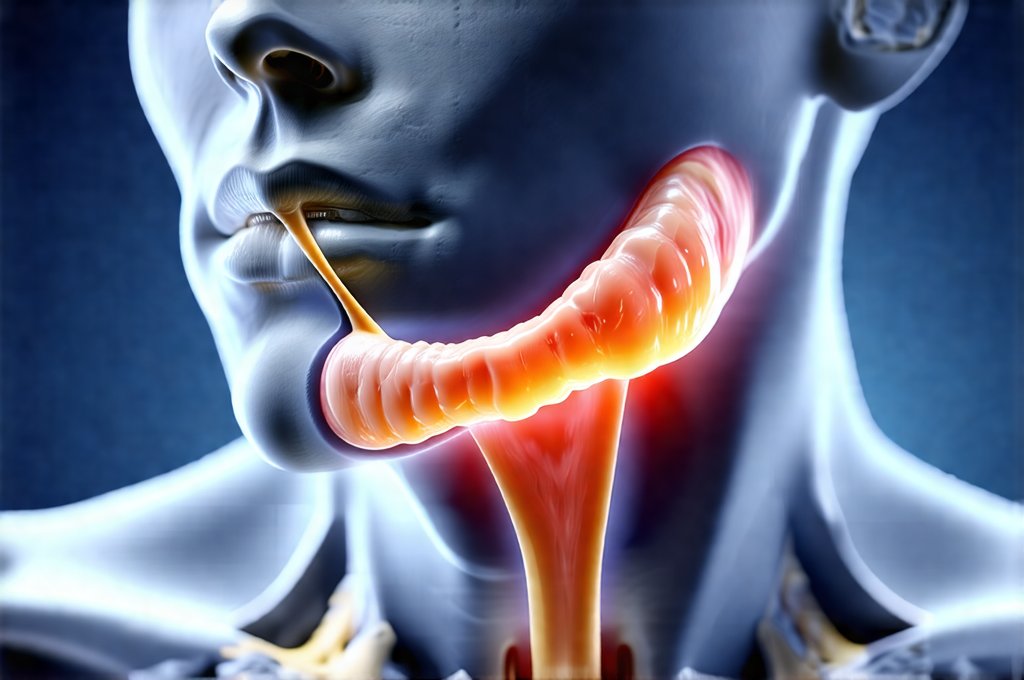
The intricate relationship between our physical and emotional states often manifests in surprising ways. Many people experience jaw tension as a symptom of stress, but few realize how deeply this tension can be connected to the digestive system, specifically the esophagus. The muscles that control chewing and facial expression are closely linked to those involved in swallowing and esophageal function, creating a biomechanical pathway where tension in one area can directly influence another. This isn’t simply about ‘stress making your jaw tight’; it’s a complex interplay of anatomy, neurology, and often, underlying emotional or psychological factors that deserve deeper understanding. Recognizing this connection is the first step towards more holistic approaches to managing discomfort and improving overall wellbeing.
The esophagus, responsible for transporting food from the mouth to the stomach, operates under significant muscular control. It isn’t a passive tube; it actively peristalses, meaning it contracts rhythmically to propel food downwards. This process requires coordinated muscle action, and any disruption – including tension originating in the jaw and surrounding muscles – can affect its efficiency. Chronic jaw tension can lead to altered swallowing patterns, increased esophageal pressure, and even contribute to symptoms often mistaken for gastrointestinal disorders. The vagus nerve, a crucial component of the gut-brain axis, plays a key role in this communication, acting as a bridge between these seemingly disparate systems. Therefore, addressing jaw tension isn’t just about relieving facial discomfort; it can be an integral part of supporting healthy esophageal function and digestive processes. Understanding the connection between stress and digestion is vital here.
The Anatomy & Neurology Linking Jaw and Esophagus
The connection begins with shared embryological origins. Structures in the head and neck region – including the jaw muscles, swallowing apparatus, and upper esophagus – develop from similar embryonic tissue. This means they share nerve supply and are intrinsically linked during development. Specifically, the trigeminal (V) and vagus (X) cranial nerves play central roles. The trigeminal nerve innervates the muscles of mastication (chewing), while the vagus nerve controls many functions within the digestive system, including esophageal motility and sensation. When the jaw is tense, signals from the trigeminal nerve can indirectly impact the vagus nerve, influencing esophageal function even without direct muscle involvement in the esophagus itself.
Furthermore, consider the hyoid bone, a small U-shaped bone in the neck that serves as an attachment point for many muscles involved in swallowing and jaw movement. Tension in the jaw muscles often pulls on the hyoid bone, affecting its position and subsequently impacting the surrounding structures including the esophagus. This altered positioning can restrict esophageal motility, potentially leading to sensations of fullness, difficulty swallowing (dysphagia), or even heartburn. It’s a subtle but significant mechanical link that highlights how localized tension can have far-reaching effects.
The temporomandibular joints (TMJs) are also integral to this interplay. Dysfunction in the TMJ – often stemming from stress, grinding teeth (bruxism), or misalignment – can radiate pain and tension throughout the head, neck, and even down into the esophagus via muscle imbalances and nerve compression. This creates a vicious cycle where jaw tension exacerbates esophageal symptoms, and vice versa. It’s important to remember that this isn’t always about obvious TMJ disorder; even mild, chronic tension can be enough to disrupt the delicate balance of these interconnected systems. Recognizing overthinking can also contribute is important as well.
Understanding Vagal Tone & Its Role
Vagal tone refers to the activity level of the vagus nerve. A high vagal tone is generally associated with better digestion, stress resilience, and emotional regulation. It indicates that the parasympathetic nervous system – responsible for ‘rest and digest’ functions – is dominant. Conversely, a low vagal tone suggests an overactive sympathetic nervous system (‘fight or flight’), often linked to increased stress, anxiety, and digestive issues. Chronic jaw tension can directly contribute to lowered vagal tone in several ways:
- Increased Sympathetic Activation: Tension activates the sympathetic nervous system, suppressing vagal activity.
- Altered Sensory Feedback: Tension disrupts normal sensory feedback from the mouth and esophagus to the brain, reducing the vagus nerve’s ability to accurately regulate digestive processes.
- Muscle Imbalance: The constant contraction of jaw muscles can create a state of chronic stress on the nervous system, diminishing its capacity for relaxation and restorative functions governed by the vagus nerve.
Restoring vagal tone is therefore often a key component in addressing both jaw tension and esophageal distress. Techniques like diaphragmatic breathing, meditation, yoga, and even gentle facial massage can all help to stimulate the vagus nerve and promote parasympathetic dominance. It’s about shifting the nervous system from a state of hyper-arousal to one of calm and balance. Understanding liver health can also support overall wellbeing.
Bruxism & Esophageal Reflux
Bruxism, or teeth grinding, is often an unconscious response to stress. While commonly associated with dental problems, it significantly exacerbates jaw tension and can directly contribute to esophageal issues. The forceful clenching and grinding create excessive pressure on the TMJs, leading to muscle imbalances and altered swallowing patterns. This can result in:
- Increased Esophageal Pressure: Bruxism alters the biomechanics of swallowing, potentially increasing pressure within the esophagus.
- Disrupted Lower Esophageal Sphincter (LES) Function: The LES is a muscular ring that prevents stomach acid from flowing back into the esophagus. Bruxism-related stress and muscle imbalances can compromise its function, leading to gastroesophageal reflux disease (GERD).
- Altered Peristalsis: The rhythmic contractions of the esophagus responsible for moving food down may be disrupted by bruxism-induced tension.
Addressing bruxism requires a multi-faceted approach. This might involve night guards provided by a dentist, stress management techniques like mindfulness or therapy, and potentially physical therapy to address muscle imbalances. It’s also important to understand the underlying cause of the bruxism – is it situational stress, anxiety, sleep disorders, or something else? – to develop a targeted treatment plan. The connection between mood and physical health shouldn’t be overlooked here either.
The Role of Swallowing Mechanics
Swallowing isn’t just about moving food; it’s a complex coordinated process involving multiple muscle groups and nerve pathways. Chronic jaw tension can disrupt the normal mechanics of swallowing in several ways:
- Altered Tongue Position: Tension often leads to an altered tongue resting position, hindering proper food manipulation and bolus formation (the ball of chewed food).
- Reduced Hyoid Bone Mobility: As mentioned earlier, jaw tension impacts the hyoid bone’s movement, affecting the timing and coordination of swallowing muscles.
- Asynchronous Muscle Activation: Tension can cause asynchronous activation of the muscles involved in swallowing, leading to inefficient clearing of food from the mouth and esophagus.
This altered swallowing pattern can contribute to several issues: – Increased risk of aspiration (food entering the airway) – Difficulty initiating a swallow – feeling like food is stuck in your throat – Increased esophageal pressure and potential for reflux symptoms – Changes in the gut microbiome due to inefficient digestion.
Speech therapists specializing in swallowing disorders (dysphagia) can provide targeted exercises to restore proper swallowing mechanics and improve muscle coordination. These exercises often focus on strengthening specific muscles, improving tongue control, and restoring a more natural rhythm to the swallow. Understanding salicylates can provide additional insight into sensitivities that impact digestion.
In conclusion, the connection between jaw tension and esophageal stress is far from coincidental. It’s a complex interplay of anatomy, neurology, and biomechanics that highlights the interconnectedness of our body systems. Addressing this connection requires a holistic approach – one that considers not only the physical symptoms but also the underlying emotional and psychological factors contributing to tension and stress. By understanding these mechanisms and adopting strategies to manage jaw tension, improve vagal tone, address bruxism, and optimize swallowing mechanics, individuals can significantly improve their digestive health and overall wellbeing. Also consider HPV screening for comprehensive gut health.