The human gut is often referred to as the “second brain,” and for good reason. It’s home to trillions of microorganisms—bacteria, fungi, viruses, and archaea—collectively known as the gut microbiome. This complex ecosystem plays a crucial role in everything from digestion and nutrient absorption to immune function and even mental health. Traditionally, assessing gut health involved limited methods like symptom tracking or basic stool tests looking for obvious pathogens. However, advancements in technology are now allowing for much deeper dives into what’s happening within our digestive system, revealing insights that were previously inaccessible. Many individuals, even those experiencing chronic symptoms, may be missing vital clues about their overall well-being simply because they aren’t utilizing or fully interpreting modern stool testing options. Understanding the importance of basic stool analysis can really help pinpoint issues.
Understanding the nuances of stool testing goes beyond just identifying “bad bugs.” It’s about painting a complete picture of gut function and microbial balance. A comprehensive approach considers not only what organisms are present, but also their relative abundance, metabolic activity, and how they interact with each other and the host (that’s you!). This article will explore some commonly overlooked aspects of stool testing, offering insights into what you might be missing and why a more detailed analysis can be invaluable for optimizing your health. We’ll focus on areas beyond basic pathogen identification, delving into markers that reveal functional imbalances and potential root causes of digestive distress or systemic symptoms. You may also want to check out what that frequent belly rub could signify.
Beyond Bacteria: The Expanding World of Microbial Analysis
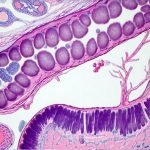
For years, stool testing largely centered around identifying the presence of pathogenic bacteria like Salmonella or E. coli. While important, this represents only a small fraction of the microbial world within our gut. Modern tests now utilize techniques like 16S rRNA gene sequencing and metagenomic sequencing to identify a much wider range of microorganisms – including fungi, viruses, and archaea – and quantify their abundance. This provides a more holistic view of the microbiome’s composition. It’s crucial to remember that the goal isn’t necessarily to eliminate all bacteria, even potentially harmful ones; it’s about balance. A healthy gut has a diverse ecosystem where beneficial microbes can outcompete pathogens, maintaining homeostasis.
Furthermore, newer testing methods are moving beyond simply identifying who is present and starting to explore what they are doing. Metatranscriptomics analyzes the RNA produced by the microbiome, revealing which genes are being expressed and what metabolic processes are actively occurring. This can provide insights into how the gut microbes are influencing digestion, immune function, and even neurotransmitter production. For instance, identifying an abundance of bacteria capable of producing hydrogen sulfide (a gas linked to inflammation) could indicate a potential source of digestive discomfort, even if no specific pathogen is identified.
Understanding fungal overgrowth is another often-missed component. While bacterial imbalances receive the most attention, Candida and other fungi can significantly disrupt gut health, leading to symptoms like bloating, brain fog, and fatigue. Traditional stool tests rarely include comprehensive fungal analysis, meaning these issues can go undetected for extended periods. Similarly, viral communities within the gut are increasingly recognized as playing a role in immune regulation and disease development, but remain largely unexplored in routine testing. If you’ve experienced food poisoning, specialized stool testing may be helpful.
Functional Markers: Assessing Gut Capabilities
Identifying what is present in the gut is only half the battle; understanding how well the gut is functioning is equally important. Comprehensive stool tests now include markers that assess various aspects of digestive capacity. These functional assessments can reveal areas where the gut may be struggling to properly break down food, absorb nutrients, or eliminate waste.
One key marker is fecal fat content. Elevated levels suggest malabsorption of fats, which could be due to insufficient pancreatic enzyme production, compromised bile acid metabolism, or damage to the intestinal lining. Similarly, assessing levels of pancreatic elastase can directly measure pancreatic function. Low levels indicate inadequate digestion of proteins and fats, potentially leading to bloating, gas, and nutrient deficiencies. Another crucial area is evaluation of inflammation. Markers like calprotectin are indicators of immune activation in the gut, suggesting inflammatory bowel disease (IBD) or other underlying conditions.
Beyond these individual markers, many tests also evaluate overall digestive capacity through parameters like short-chain fatty acid (SCFA) production. SCFAs – acetate, propionate, and butyrate – are produced by bacteria fermenting fiber in the colon and provide numerous health benefits, including nourishing gut cells and reducing inflammation. Low SCFA levels can indicate a lack of beneficial bacteria or insufficient fiber intake. Optimizing digestive function is fundamental to overall health, and these functional markers offer valuable insights into potential areas for improvement. Understanding how stool testing fits into long-term care is also key.
The Role of Bile Acids
Bile acids are essential for the digestion and absorption of fats, as well as the elimination of cholesterol. They are produced by the liver and released into the small intestine during meals. Gut bacteria play a significant role in modifying bile acids, influencing their reabsorption and overall impact on health. Stool testing can now assess bile acid profiles, revealing imbalances that may contribute to digestive issues or systemic problems.
- Dysbiosis – an imbalance in gut microbiota – can disrupt bile acid metabolism, leading to altered ratios of primary and secondary bile acids.
- Impaired bile acid deconjugation (the process of removing amino acids from bile acids) can reduce their effectiveness in fat digestion and increase the risk of diarrhea.
- An overgrowth of certain bacteria can lead to excessive deconjugation, resulting in bile acid diarrhea – a common symptom experienced by individuals with SIBO (Small Intestinal Bacterial Overgrowth).
Identifying these imbalances allows for targeted interventions like dietary adjustments, supplementation with digestive enzymes, or strategies to support healthy gut microbial composition. Addressing bile acid metabolism is often overlooked but can have a profound impact on digestion and overall well-being.
Understanding Secretory IgA (sIgA)
Secretory IgA is an antibody produced by the immune cells in the gut lining. It acts as a first line of defense against pathogens, preventing them from adhering to the intestinal wall and causing infection. Measuring sIgA levels in stool provides valuable information about the integrity of the gut’s immune barrier.
- Low sIgA levels indicate a weakened immune function in the gut, making individuals more susceptible to infections and inflammation. This can be caused by factors like stress, poor diet, or chronic illness.
- Elevated sIgA levels may suggest ongoing inflammation or an overactive immune response, potentially indicating food sensitivities or autoimmune activity.
- Assessing sIgA alongside other markers, such as calprotectin, provides a more nuanced understanding of the gut’s immune status and can guide targeted interventions to support immune function.
It is important to note that sIgA levels can fluctuate based on various factors, so interpreting results requires considering the individual’s overall health context and symptoms.
The Impact of Parasitic Infections
While often associated with developing countries, parasitic infections are surprisingly common even in developed nations. Traditional stool tests frequently utilize methods like O&P (ova and parasite) exams, which can be limited in their sensitivity and ability to detect all parasites. Modern testing employs more advanced techniques like PCR (polymerase chain reaction) to identify parasitic DNA with greater accuracy.
- Many parasitic infections are asymptomatic or present with vague symptoms like fatigue, digestive upset, or muscle aches, making them difficult to diagnose without specific testing.
- Common parasites like Giardia, Cryptosporidium, and Blastocystis hominis can disrupt gut health, leading to inflammation, malabsorption, and altered microbial balance.
- Co-infections (multiple parasitic infections occurring simultaneously) are also common and require comprehensive testing for accurate diagnosis and treatment.
Identifying and addressing parasitic infections is crucial for restoring gut health and alleviating associated symptoms. It’s important to work with a healthcare professional experienced in treating these types of infections, as treatment protocols can vary depending on the parasite involved. Recognizing stool signs during routine checks is vital.
Ultimately, modern stool testing offers a powerful tool for understanding the intricate workings of the digestive system. By going beyond basic pathogen identification and embracing functional markers, we can gain invaluable insights into gut health and identify potential root causes of symptoms that might otherwise remain elusive. It’s about moving from reactive symptom management to proactive health optimization—using data-driven insights to nourish our microbiome and unlock our full potential for well-being. Many individuals may be experiencing undiagnosed silent reflux without realizing it.