Chronic inflammation is increasingly recognized as a central driver in many prevalent diseases, ranging from autoimmune conditions like inflammatory bowel disease (IBD) and rheumatoid arthritis to cardiovascular disease, type 2 diabetes, and even neurodegenerative disorders. Traditionally, assessing long-term inflammation has relied heavily on blood tests – measuring markers like C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and various cytokines. However, blood provides a systemic snapshot that doesn’t always accurately reflect what’s happening locally within the gut, often considered a major site of chronic inflammation for many individuals. Moreover, blood tests can be influenced by factors beyond intestinal inflammation, leading to potential inaccuracies or requiring invasive procedures like colonoscopies for definitive diagnosis and monitoring.
The gastrointestinal tract presents an ideal location for non-invasive assessment of inflammation due to its direct contact with the luminal environment and its significant role in immune function. Stool samples offer a unique window into gut health, reflecting the interplay between the host’s immune system, the gut microbiome, and dietary components. Increasingly sophisticated stool-based tests are emerging as valuable tools for monitoring chronic inflammation, offering advantages over traditional methods in terms of convenience, cost-effectiveness, and ability to capture localized inflammatory processes. This article will explore the various options available for utilizing stool analysis to monitor long-term inflammation, outlining their strengths, limitations, and potential applications.
Stool Biomarkers of Inflammation
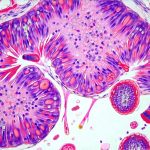
The cornerstone of stool-based inflammation monitoring lies in identifying specific biomarkers that are released during intestinal inflammatory responses. Fecal calprotectin is arguably the most well-established and widely used marker. It’s a calcium-binding protein released by neutrophils (a type of white blood cell) when activated, indicating intestinal inflammation. Elevated fecal calprotectin levels are strongly associated with IBD – Crohn’s disease and ulcerative colitis – and can help differentiate between inflammatory and non-inflammatory bowel conditions like irritable bowel syndrome (IBS). Importantly, it’s not specific to IBD; other sources of gut inflammation can also elevate calprotectin levels.
Beyond fecal calprotectin, researchers are investigating several other promising stool biomarkers. Lactoferrin, another neutrophil-derived protein, is often measured alongside calprotectin to improve diagnostic accuracy. Fecal matrix metalloproteinase-9 (MMP-9) is an enzyme released during tissue breakdown in inflammation and shows promise as a marker of disease activity, particularly in ulcerative colitis. Newer approaches are even looking at the stool microbiome composition itself as an indicator of inflammation – specifically, alterations in microbial diversity and abundance of certain bacterial species associated with inflammatory states. The concept here isn’t necessarily to identify specific pathogens but rather to understand how imbalances within the gut microbiome contribute to chronic inflammation. How to Reduce Inflammation Through Nutrition can offer valuable insights into dietary approaches. It’s crucial to remember that interpreting stool biomarker results requires clinical context. A single elevated reading doesn’t automatically confirm a diagnosis; it necessitates correlation with patient symptoms, medical history, and other diagnostic tests. Furthermore, pre-analytical factors like collection methods, storage conditions, and laboratory assays can influence biomarker levels, emphasizing the need for standardized protocols to ensure reliable results.
Advanced Stool Analysis Techniques
While traditional stool biomarker measurements are valuable, advanced techniques are broadening our understanding of gut inflammation at a molecular level. Metagenomics, also known as 16S rRNA gene sequencing or whole-genome shotgun metagenomics, allows for comprehensive analysis of the microbial communities present in the stool sample. This provides insights into the diversity, composition, and functional potential of the gut microbiome. Changes in microbial populations – such as a decrease in beneficial bacteria like Faecalibacterium prausnitzii and an increase in pro-inflammatory species – can indicate ongoing inflammation.
Another emerging technology is metabolomics, which focuses on identifying and quantifying the small molecules (metabolites) produced by gut microbes and host cells. Metabolomic analysis can reveal alterations in metabolic pathways associated with inflammation, providing a more nuanced understanding of disease processes. For example, changes in short-chain fatty acids (SCFAs), like butyrate – known for their anti-inflammatory properties – can indicate disruptions in microbial metabolism and gut health. Combining metagenomics and metabolomics—a multi-omics approach—is particularly powerful, providing a holistic view of the interplay between microbes, metabolites, and host inflammation. Strategies to Prevent Pancreatic Inflammation highlights preventative measures relevant to overall gut health. These advanced analyses are still largely research tools but are gradually becoming more accessible for clinical applications. The challenge lies in translating complex multi-omic data into actionable insights for patient care. Developing robust algorithms and standardized protocols is essential to ensure accurate interpretation and reliable results.
Assessing Gut Permeability & Inflammation
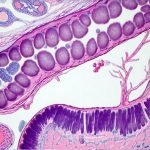
Gut permeability, often referred to as “leaky gut,” plays a significant role in chronic inflammation. When the intestinal barrier becomes compromised, larger molecules can pass through into the bloodstream, triggering an immune response and systemic inflammation. Stool-based tests are beginning to offer indirect assessments of gut permeability, although direct measurement remains challenging. Zonulin, a protein released by intestinal cells in response to stress or microbial imbalances, is one marker gaining attention. Elevated zonulin levels in stool suggest increased intestinal permeability.
However, it’s important to note that the relationship between zonulin and gut permeability is complex and still under investigation. Zonulin isn’t necessarily a direct measure of barrier function but rather an indicator of its activation. More advanced research focuses on quantifying specific metabolites indicative of barrier dysfunction – such as lactulose and mannitol – following oral administration in what’s called a “lactulose-mannitol test.” These sugars are absorbed differently depending on gut permeability, allowing for an estimation of intestinal integrity.
Furthermore, the microbiome itself significantly impacts gut barrier function. Microbial dysbiosis can contribute to increased permeability, while beneficial bacteria promote barrier integrity by producing SCFAs and strengthening tight junctions between intestinal cells. Therefore, integrating stool-based microbiome analysis with assessments of gut permeability provides a more comprehensive picture of intestinal health and inflammation. Can Gut Inflammation Lead to Weight Gain and Bloating? explores the systemic effects of compromised gut function.
Inflammatory Cytokine & Metabolite Profiles
While fecal calprotectin remains the gold standard, analyzing specific inflammatory cytokines within stool samples is gaining traction. Although cytokine levels in stool are generally lower than those found in blood, advancements in sensitive detection methods – like ELISA (enzyme-linked immunosorbent assay) and multiplex assays – are making it feasible to quantify key pro-inflammatory cytokines such as tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6). This provides a direct measure of the inflammatory response occurring within the gut lumen.
Simultaneously, characterizing the stool metabolome can reveal valuable insights into inflammatory processes. Identifying elevated levels of pro-inflammatory metabolites – like lipopolysaccharide (LPS), a component of bacterial cell walls – or decreased levels of anti-inflammatory metabolites – such as SCFAs – provides clues about the underlying mechanisms driving inflammation. Genetic Predisposition to Lactose Intolerance: Testing options can help identify individual sensitivities impacting gut health. Tryptophan metabolism is another area of intense research, with specific tryptophan metabolites reflecting gut microbial activity and immune modulation.
The challenge here lies in understanding the complex interplay between cytokines, metabolites, and the microbiome. A holistic approach that integrates these different data points – along with clinical information – is essential for accurate interpretation and personalized treatment strategies. Is It Safe to Take Antacids Long-Term for GERD? addresses common interventions in digestive health.
Personalized Monitoring & Therapeutic Guidance
Ultimately, the goal of stool-based inflammation monitoring isn’t just diagnosis but also personalized therapeutic guidance. By tracking changes in biomarker levels over time, clinicians can assess a patient’s response to interventions like dietary modifications, probiotic supplementation, or pharmacological therapies. For example, a decrease in fecal calprotectin following a change in diet suggests improved gut health and reduced inflammation.
The increasing availability of at-home stool collection kits is making long-term monitoring more convenient for patients. This allows for frequent assessments, providing a dynamic picture of intestinal inflammation and enabling timely adjustments to treatment plans. However, it’s crucial that these tests are conducted under the guidance of a healthcare professional to ensure accurate interpretation and appropriate follow-up. How to Manage Long-Term Side Effects of Cancer Treatment offers insights into managing chronic conditions affecting gut health.
Looking ahead, artificial intelligence (AI) and machine learning algorithms will likely play an increasingly important role in analyzing complex stool data and predicting individual responses to therapy. This could lead to highly personalized interventions tailored to each patient’s unique gut microbiome and inflammatory profile—a future where stool analysis is not just a diagnostic tool but a cornerstone of proactive, preventative healthcare. How to Reduce Inflammation Through Nutrition emphasizes the power of dietary interventions for managing inflammation.