Inflammation within the digestive tract, often referred to as gut inflammation, is a surprisingly common underlying factor in a wide range of health issues. It’s not always obvious – it doesn’t necessarily present with dramatic symptoms like severe abdominal pain (though it can!). Instead, it frequently manifests as more subtle problems such as bloating, fatigue, changes in bowel habits, or even skin conditions. Understanding how doctors assess for gut inflammation is the first step towards addressing potential issues and improving overall health. The gut is a complex ecosystem, and identifying where and why inflammation exists requires careful evaluation using a variety of tools, ranging from simple questions about your symptoms to sophisticated laboratory tests.
The diagnostic process isn’t usually about finding inflammation itself; it’s about uncovering the cause of that inflammation. Is it related to infection, autoimmune activity, food sensitivities, or something else entirely? Doctors aim to differentiate between acute (short-term) and chronic (long-term) inflammation, as this significantly impacts treatment approaches. Furthermore, pinpointing the location within the gut – is it in the stomach, small intestine, or colon? – is crucial for accurate diagnosis and effective management. This article will explore some of the simple, yet powerful, ways physicians check for signs of gut inflammation, offering insight into what to expect during assessment and why these tests are used.
Initial Assessment & Patient History
The first line of defense in checking for gut inflammation often begins with a thorough conversation between you and your doctor. This isn’t just about listing symptoms; it’s about building a comprehensive picture of your overall health and lifestyle. Doctors will ask detailed questions about your medical history, including any existing conditions, previous surgeries, medications you’re taking (including over-the-counter drugs and supplements), and family history of gastrointestinal diseases like Crohn’s disease or ulcerative colitis. They’ll also inquire about your diet, stress levels, and lifestyle habits such as smoking and alcohol consumption. A detailed patient history is often the most valuable diagnostic tool available. Understanding how [strategic meal layers] (https://vitagastro.com/strategic-meal-layers-that-prevent-food-conflict-in-the-gut/) can impact your gut health is also important during this stage.
Beyond general health questions, specific inquiries will focus on the nature of your digestive symptoms. This includes: – Frequency and consistency of bowel movements – Presence of blood or mucus in stool – Abdominal pain (location, severity, type) – Bloating, gas, and heartburn – are they constant or intermittent? – Nausea and vomiting – Unintentional weight loss – Extraintestinal symptoms, such as skin rashes, joint pain, or fatigue. These seemingly unrelated symptoms can sometimes point to underlying gut inflammation. If you suspect issues related to bloating, exploring [gut biofeedback] (https://vitagastro.com/the-role-of-gut-biofeedback-in-managing-chronic-bloating/) might provide valuable insights.
This initial assessment provides crucial clues about potential causes of inflammation and guides the selection of further diagnostic tests. It helps narrow down possibilities and ensures that testing is targeted and efficient. A doctor might suspect inflammatory bowel disease (IBD) based on chronic diarrhea, abdominal pain, and weight loss, while food sensitivities may be suspected if symptoms consistently arise after eating specific foods. It’s important to be as honest and detailed as possible when answering these questions; even seemingly insignificant details can be helpful in the diagnostic process. Considering [digestive rest days] (https://vitagastro.com/the-role-of-digestive-rest-days-for-gut-recovery/) during periods of digestive distress can also support healing.
Stool Tests: A Window into the Gut
Stool tests are a non-invasive yet powerful tool for detecting inflammation and identifying potential causes. They can reveal information about infections, bleeding, malabsorption, and gut microbiome imbalances. There are several types of stool tests commonly used to assess gut health.
One frequently ordered test is the fecal calprotectin test. Calprotectin is a protein released by white blood cells when inflammation occurs in the intestines. Elevated levels of fecal calprotectin strongly suggest intestinal inflammation and can help differentiate between IBD (inflammatory bowel disease) and irritable bowel syndrome (IBS), where calprotectin levels are typically normal. Another common stool test looks for occult (hidden) blood, which may indicate bleeding from ulcers or polyps in the digestive tract – often a sign of inflammation or other issues. Detecting occult blood is not necessarily indicative of IBD but warrants further investigation. If you notice signs of fermentation leading to painful pressure, understanding [fermentation in the gut] (https://vitagastro.com/why-fermentation-in-the-gut-causes-painful-pressure/) can be beneficial.
Beyond these specific markers, comprehensive stool analysis can provide detailed information about the gut microbiome – the trillions of bacteria and other microorganisms that live in your digestive tract. Imbalances in the microbiome (dysbiosis) are often linked to inflammation and various health problems. Stool tests can identify specific bacterial species present, detect parasitic infections, and assess levels of beneficial and harmful bacteria. These results help tailor dietary recommendations and probiotic therapies to restore a healthy gut ecosystem. Learning [how to train the gut] (https://vitagastro.com/how-to-train-the-gut-for-better-tolerance-to-fiber/) for better fiber tolerance is also crucial in supporting microbiome health.
Blood Tests: Inflammatory Markers & Beyond
Blood tests play a vital role in assessing for systemic inflammation and identifying potential causes of gut issues. While stool tests reveal what’s happening within the digestive tract, blood tests provide insights into the body’s overall inflammatory response and can help rule out other conditions with similar symptoms. Several key markers are commonly measured: – C-reactive protein (CRP) – a general marker of inflammation throughout the body. Elevated CRP levels suggest inflammation but don’t necessarily pinpoint its location. – Erythrocyte sedimentation rate (ESR) – another nonspecific marker of inflammation, often used in conjunction with CRP.
More specifically, blood tests can help identify autoimmune activity, which is a common cause of chronic gut inflammation. Tests for antibodies associated with conditions like celiac disease or IBD can provide valuable diagnostic information. For instance, anti-tissue transglutaminase (tTG) and endomysial antibody tests are used to diagnose celiac disease, an autoimmune reaction triggered by gluten ingestion. Similarly, tests for anti-neutrophil cytoplasmic antibodies (ANCA) and anti-Saccharomyces cerevisiae antibodies (ASCA) can assist in differentiating between Crohn’s disease and ulcerative colitis.
Furthermore, blood tests assess nutritional status. Malabsorption due to gut inflammation can lead to deficiencies in essential vitamins and minerals like iron, vitamin B12, and vitamin D. Identifying these deficiencies is crucial for appropriate supplementation and restoring overall health. A complete blood count (CBC) can also reveal signs of anemia or infection, further guiding the diagnostic process. Blood tests provide a broader picture of systemic health and inflammation. If you suspect histamine reaction in your gut, blood testing can help identify this issue.
Endoscopy & Colonoscopy: Direct Visualization
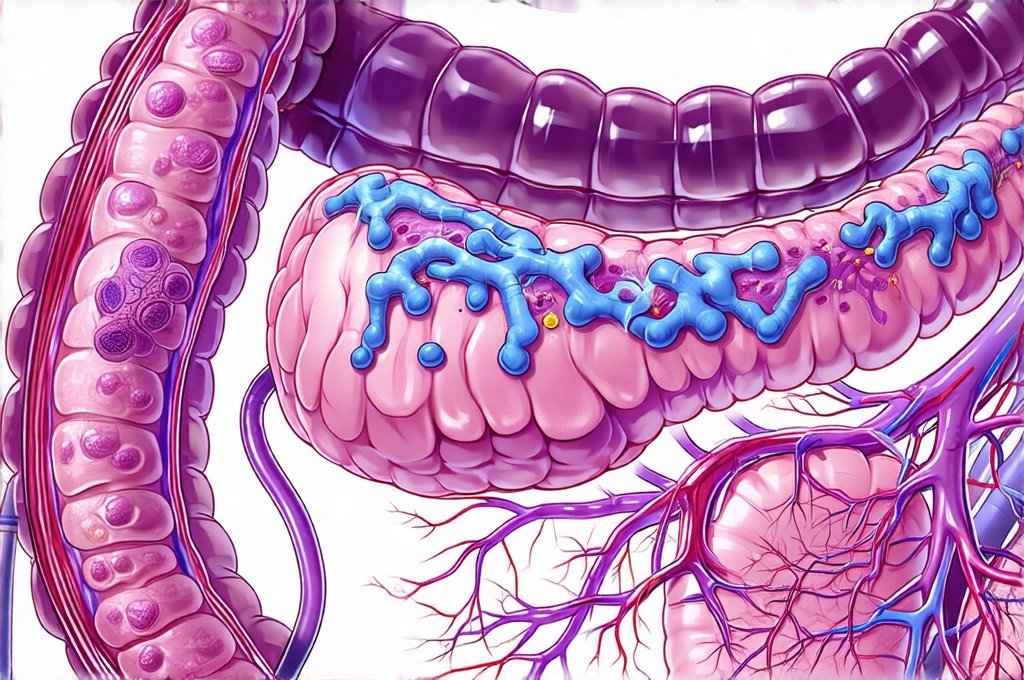
While less “simple” than stool or blood tests, endoscopy and colonoscopy are often necessary for accurate diagnosis and assessment of gut inflammation. These procedures involve inserting a flexible tube with a camera attached into the digestive tract to directly visualize the lining of the esophagus, stomach, small intestine (endoscopy), or colon (colonoscopy). This allows doctors to identify areas of inflammation, ulcers, polyps, or other abnormalities.
During an endoscopy, biopsies – small tissue samples – can be taken from suspicious areas and examined under a microscope for signs of inflammation, infection, or cancer. Similarly, during a colonoscopy, biopsies are often performed to confirm diagnoses like IBD or colorectal cancer. Colonoscopies are particularly important for screening purposes, as they can detect precancerous polyps that can be removed before developing into cancer. These procedures are considered invasive but offer unparalleled diagnostic accuracy.
Before undergoing these procedures, patients typically need to prepare their digestive tract through bowel preparation (for colonoscopy) or fasting (for endoscopy). While the preparations can be uncomfortable, they are essential for ensuring clear visualization and accurate results. Endoscopy and colonoscopy are valuable tools for confirming diagnoses, assessing disease severity, and monitoring treatment effectiveness. They allow doctors to directly assess the extent of inflammation and guide appropriate management strategies.