Digestive scar tissue, often resulting from surgeries, inflammation (like Crohn’s disease or ulcerative colitis), radiation therapy, or even previous infections, can silently disrupt normal gastrointestinal function. It’s not always immediately apparent – symptoms can be vague and easily attributed to other causes, making diagnosis challenging. This internal ‘stickiness’, known medically as adhesion, isn’t typically visible on standard imaging tests, leading many patients to suffer for years with unexplained abdominal pain, bloating, bowel obstruction, or infertility (in women, adhesions can affect reproductive organs). Understanding the methods available to detect this hidden scar tissue is crucial for accurate diagnosis and appropriate management.
The challenge lies in the nature of adhesions themselves. They are often thin, filmy bands of collagenous tissue that blend with surrounding structures, making them difficult to differentiate from normal anatomy using conventional imaging. Furthermore, the location can vary greatly – they might form between loops of bowel, between the bowel and abdominal wall, or even around other organs. This article will explore the various scanning technologies employed to identify these adhesions, their strengths and weaknesses, and what patients can expect during these investigations. It’s important to remember that no single scan is perfect; often a combination of techniques and clinical evaluation are required for accurate assessment. Considering hidden signs can be the first step towards understanding digestive issues.
Identifying Adhesions: A Spectrum of Imaging Techniques
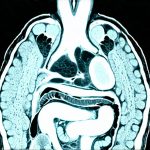
Traditional imaging methods like X-rays and standard CT scans frequently miss adhesions due to their subtle nature. However, advancements in imaging technology have provided clinicians with more sophisticated tools. Magnetic Resonance Imaging (MRI) has emerged as a particularly valuable modality, offering superior soft tissue detail compared to CT scans. A specialized MRI protocol focusing on the abdomen and pelvis can often visualize adhesions, especially those causing significant obstruction or impacting other organs. The key is high-resolution imaging and careful interpretation by a radiologist experienced in gastrointestinal disorders.
Beyond standard MRI, techniques like diffusion-weighted imaging (DWI) are becoming increasingly utilized. DWI measures the movement of water molecules within tissues; adhesions typically exhibit restricted water diffusion compared to healthy tissue, making them more visible on these scans. Another promising technique is MR enterography which involves drinking a liquid contrast agent that highlights the small intestine, allowing for better visualization of potential obstructions or narrowing caused by adhesions. While MRI provides excellent detail, it can be time-consuming and may not be suitable for all patients (e.g., those with certain metallic implants). Tests connecting digestive issues to neurological symptoms are also important to consider.
CT scans, while less sensitive than MRI for detecting subtle adhesions, still play a role, particularly when combined with specific techniques. A CT enterography utilizes oral contrast to visualize the small bowel, similar to MR enterography, allowing radiologists to identify areas of narrowing or obstruction that may indicate adhesive disease. Importantly, contrast-enhanced CT scans can help differentiate between fluid-filled loops of bowel and solid adhesions, improving diagnostic accuracy. The choice between MRI and CT often depends on individual patient factors, clinical presentation, and the availability of specialized imaging protocols. When preparing for potential surgery, digestive tests are vital.
Understanding Hydrographic Studies (Small Bowel Follow-Through)
A hydrographic study, also known as a small bowel follow-through, is an older but sometimes still valuable technique for assessing intestinal obstruction caused by adhesions. It involves swallowing a barium solution that coats the digestive tract and then taking X-ray images to track its passage through the small intestine. Adhesions can cause narrowing or complete blockage of the bowel, leading to delayed transit or pooling of barium in specific areas.
- The procedure typically takes several hours as radiologists observe the barium’s movement.
- It’s less invasive than many other imaging modalities but provides limited detail regarding the specific nature of the obstruction – it can confirm a blockage exists, but not necessarily pinpoint its cause definitively.
- While useful for identifying significant obstructions, hydrographic studies are generally less effective at detecting subtle or early-stage adhesive disease. Furthermore, barium exposure should be considered, particularly in pregnant women or children. Addressing urgent bowel movements can help rule out other causes.
Laparoscopy: The Gold Standard for Diagnosis
While imaging techniques have improved significantly, laparoscopy remains the gold standard for diagnosing intra-abdominal adhesions. This minimally invasive surgical procedure involves inserting a small camera (laparoscope) through tiny incisions in the abdomen to directly visualize the internal organs and identify any adhesive bands. It’s often used when imaging studies are inconclusive or to assess the extent of adhesion-related disease before surgery is planned.
- The patient undergoes general anesthesia.
- Small incisions are made, typically around the navel.
- A laparoscope and surgical instruments are inserted through these incisions.
- The surgeon visually inspects the abdominal cavity for adhesions.
Laparoscopy not only allows for diagnosis but also provides an opportunity to surgically release (lyse) adhesions during the same procedure, relieving symptoms and restoring bowel function. However, it is a surgical procedure with inherent risks, and its use should be carefully considered based on the patient’s clinical condition and imaging findings. It’s generally reserved for situations where diagnosis is uncertain or when surgical intervention is likely to be required. Small wins in managing digestive health can often delay the need for such interventions.
The Role of Virtual Colonoscopy & Emerging Technologies
Virtual colonoscopy (CT colonography) isn’t typically used specifically to detect adhesions, as its primary focus is the large intestine and rectum. However, it can sometimes incidentally identify abnormalities in the surrounding abdominal structures that might suggest adhesive disease. This technology uses a CT scan to create a 3D reconstruction of the colon, allowing for detailed visualization without the need for direct insertion of a scope.
Beyond established imaging techniques, research is ongoing into novel technologies for detecting adhesions. These include:
– Ultrasound elastography which assesses tissue stiffness – adhesions tend to be stiffer than normal bowel wall.
– Advanced MRI sequences with specialized contrast agents designed to highlight areas of inflammation or fibrosis (scarring).
– Artificial intelligence (AI) algorithms that can analyze imaging data and identify subtle patterns indicative of adhesive disease. These are still in early stages of development but hold promise for improving diagnostic accuracy and efficiency. Many find relief through herbal remedies to alleviate some symptoms.
It’s essential to remember that the investigation of potential digestive scar tissue is a collaborative process between patient, physician, and radiologist. A thorough clinical evaluation combined with appropriate imaging studies tailored to individual circumstances will lead to the most accurate diagnosis and effective management plan.