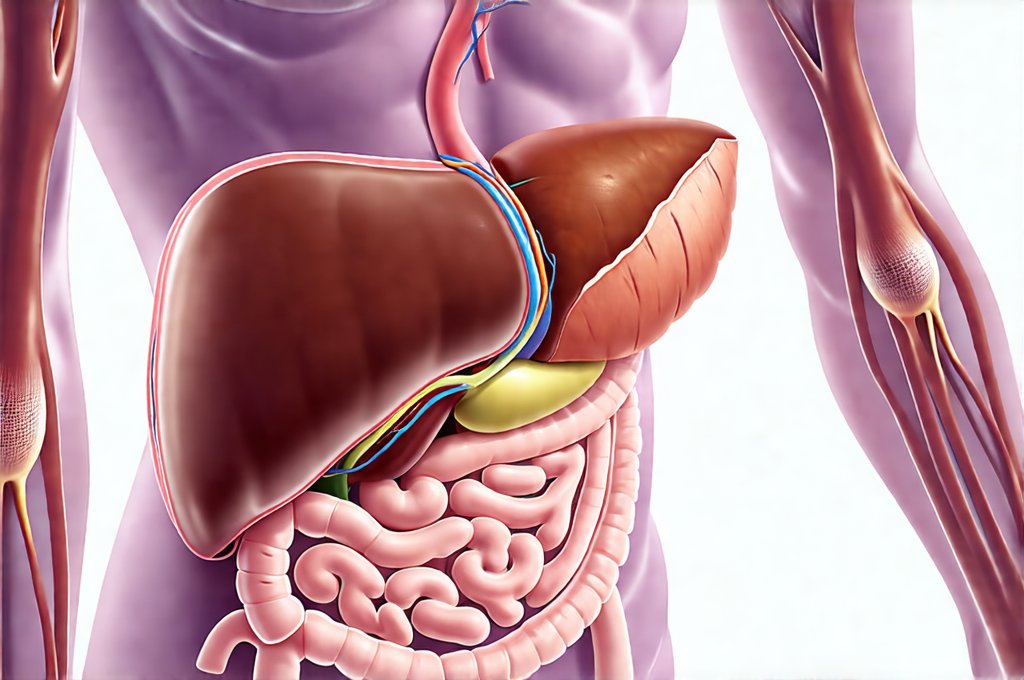
The liver plays an absolutely critical role in digestion, far beyond simply processing what we eat. It manufactures bile, essential for fat breakdown and absorption, metabolizes nutrients from food, detoxifies harmful substances, and stores vital vitamins and minerals. When the liver isn’t functioning optimally, or when there are underlying issues affecting its ability to perform these tasks, it can manifest as a wide range of digestive problems – from bloating and nausea to chronic diarrhea and severe malabsorption. Recognizing these issues early is paramount for effective management, but pinpointing the source of the problem often requires careful investigation using various scan and test options.
Digestive symptoms related to liver dysfunction are frequently subtle at first, making diagnosis challenging. Many individuals attribute initial discomfort to dietary choices or stress, overlooking the potential involvement of this vital organ. Conditions like non-alcoholic fatty liver disease (NAFLD) and chronic hepatitis can develop silently for years before becoming symptomatic, while acute issues like biliary obstruction present with more immediate and noticeable distress. This highlights the need for proactive assessment, particularly for individuals at risk due to factors such as obesity, diabetes, excessive alcohol consumption, or a family history of liver disease. Understanding available scan and test options empowers patients to engage in informed conversations with their healthcare providers and take control of their digestive health journey. Consider also exploring steady digestion eating templates for support.
Imaging Scans for Liver Assessment
Imaging scans are often the first line of defense in assessing potential liver-related digestion problems. They provide visual information about the structure of the liver, gallbladder, and bile ducts, helping to identify abnormalities such as tumors, cysts, stones, or signs of inflammation. The choice of scan depends on the specific symptoms and suspected underlying cause. Ultrasound is frequently used as an initial screening tool due to its non-invasive nature and relatively low cost. It utilizes sound waves to create images of the liver and surrounding structures, making it effective for detecting gallstones, fatty liver disease, and some types of tumors. However, ultrasound image quality can be affected by body habitus and gas in the intestines.
More detailed imaging options include computed tomography (CT) scans and magnetic resonance imaging (MRI). CT scans use X-rays to create cross-sectional images, providing a comprehensive view of the liver and surrounding organs. MRI uses magnetic fields and radio waves, offering even greater detail and the ability to differentiate between different types of tissue without using radiation. MRI is often preferred for evaluating tumors and bile duct abnormalities as it offers superior soft tissue contrast. These scans may require intravenous contrast dye, which can have potential risks, so it’s important to discuss these with your doctor beforehand.
Finally, specialized imaging techniques like MRCP (magnetic resonance cholangiopancreatography) provide detailed views of the biliary ducts and pancreatic duct, helping to identify blockages or narrowing caused by stones, tumors, or inflammation. This technique doesn’t require invasive procedures and is often used as an alternative to endoscopic retrograde cholangiopancreatography (ERCP), which carries a higher risk of complications. The selection of appropriate imaging will be determined based on the individual patient’s clinical presentation and medical history. If you have concerns about colorectal health, screening options are available.
Blood Tests for Liver Function Evaluation
Blood tests are essential companions to imaging scans, providing functional information about the liver’s ability to perform its various tasks. Liver function tests (LFTs) measure levels of enzymes released by liver cells when damaged, as well as substances processed by the liver like bilirubin and albumin. Elevated levels of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) suggest liver cell damage, while elevated bilirubin can indicate problems with bile excretion or processing. A low level of albumin may signal chronic liver disease affecting protein synthesis.
Beyond basic LFTs, more specific blood tests can help pinpoint the cause of liver dysfunction. These include:
– Tests for viral hepatitis (A, B, C) to identify infectious causes.
– Autoimmune markers to assess autoimmune hepatitis.
– Ceruloplasmin and copper levels to evaluate Wilson’s disease, a genetic disorder affecting copper metabolism.
– Iron studies to screen for hemochromatosis, another genetic condition leading to iron overload.
It’s important to remember that LFT results should be interpreted in context with the patient’s symptoms, medical history, and other test findings. Abnormal results don’t automatically equate to liver disease; they often indicate a need for further investigation. For example, mildly elevated ALT levels can occur due to muscle injury or strenuous exercise. Further testing like stool tests may be necessary.
Stool Analysis: Detecting Bile Acid Malabsorption
Bile acid malabsorption (BAM) is a frequently overlooked cause of chronic diarrhea and digestive discomfort that’s strongly linked to liver function. When the liver doesn’t produce enough bile, or when there’s a blockage preventing its flow, fats aren’t properly digested, leading to steatorrhea (fatty stools). Furthermore, unabsorbed bile acids can irritate the colon, causing diarrhea, bloating, and abdominal pain. Stool analysis specifically looking for elevated levels of fecal bile acids can confirm BAM.
There are two primary methods for assessing BAM:
1. Fecal Bile Acid Quantification: This involves measuring the concentration of total bile acids in a stool sample. Elevated levels suggest malabsorption. The accuracy and reliability of this method can vary depending on collection techniques and laboratory protocols.
2. SeHCAT Scan (Selenium Homotaurine Cholate): A more sophisticated test, the SeHCAT scan involves swallowing a small amount of radioactive selenium-labeled bile acid compound. After 7 days, a scan is performed to measure how much of the compound has been excreted in the stool, indicating how well bile acids are being absorbed. This method provides a more accurate assessment of BAM and can help differentiate between different causes of diarrhea.
Identifying BAM is crucial because treatment with bile acid sequestrants – medications that bind to bile acids in the intestine – can significantly alleviate symptoms. Addressing BAM often improves digestion and quality of life for those affected by liver-related digestive issues. A hydrogen breath test might also help diagnose underlying causes. Also consider post-indulgence food options to aid recovery.
It’s vital to reiterate, this information is intended for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.