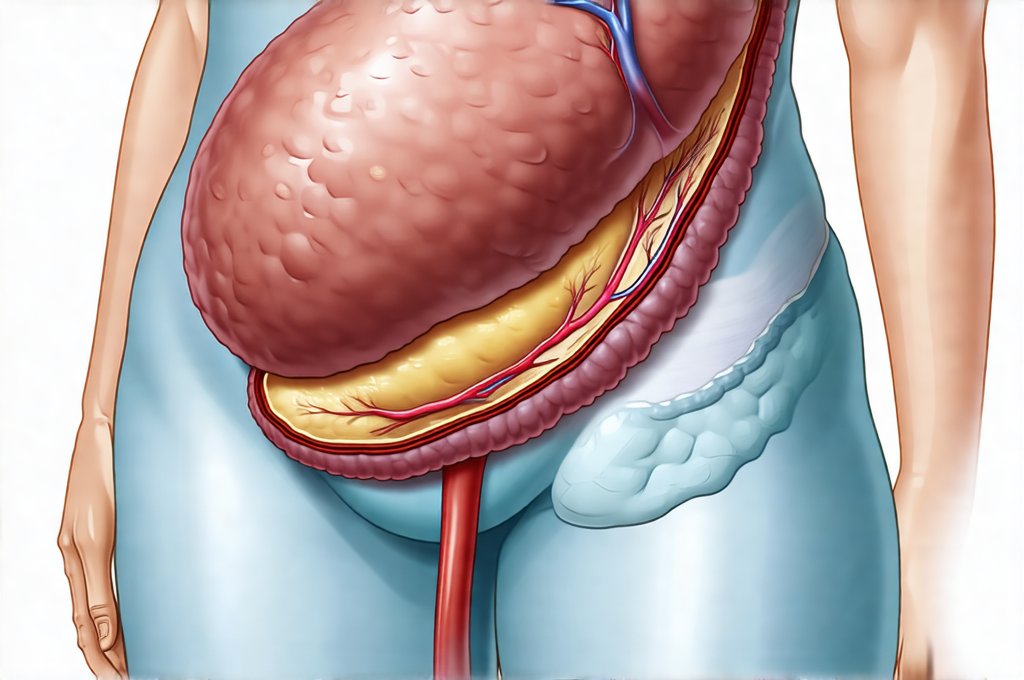
Gallbladder removal, known as cholecystectomy, is a very common surgical procedure often performed to alleviate symptoms caused by gallstones or other gallbladder diseases. While generally considered safe and effective, removing the gallbladder can alter how your body digests fats, potentially leading to changes in bowel habits or digestive discomfort for some individuals. Understanding what follow-up care and testing might be recommended after surgery is crucial for ensuring a smooth recovery and addressing any potential complications proactively. This isn’t about anticipating problems, but rather being prepared and informed about maintaining long-term health following this significant change.
Post-cholecystectomy life is usually positive for most people. However, the gallbladder plays a role in storing bile, which aids in fat digestion. When it’s removed, bile flows directly from the liver to the small intestine, sometimes leading to adjustments your body needs to make. Routine check-ins with your healthcare provider and potentially some targeted testing can help identify these changes early on and allow for appropriate management strategies. It’s important to remember that every individual responds differently to gallbladder removal; what one person experiences isn’t necessarily indicative of another’s journey, so personalized follow-up is key. Understanding how gallbladder removal influences gas and digestion can be very helpful during this time.
Understanding Post-Cholecystectomy Symptoms & Follow-Up
The initial recovery period after a cholecystectomy typically involves managing pain and wound care as directed by your surgeon. However, even after the immediate post-operative phase, many patients experience ongoing digestive changes. These are often temporary as the body adjusts to life without a gallbladder. Common symptoms can include: – Bloating – Diarrhea – Gas – Abdominal discomfort – particularly after eating fatty foods. These postcholecystectomy syndrome symptoms are generally mild and resolve within a few weeks or months, but persistent or severe symptoms warrant further investigation. Follow-up appointments with your surgeon and potentially a gastroenterologist will be scheduled to monitor your progress and address any concerns. These appointments aren’t just about reacting to problems; they’re an opportunity for education about dietary adjustments and lifestyle modifications that can optimize digestive health. Consider restorative meal ideas as you adjust.
The type of follow-up testing recommended often depends on the individual’s symptoms and overall health. A standard initial check-up will involve a discussion of your symptoms, diet, and bowel habits. Your doctor may also inquire about any medications you’re taking, as some medications can interact with bile acid absorption or exacerbate digestive issues. Further investigations are usually triggered by persistent symptoms that don’t improve with dietary changes or over-the-counter remedies. This is where the selection of specific tests comes into play – it’s not a one-size-fits-all approach but tailored to your individual presentation.
The goal isn’t simply to detect something wrong, but rather to understand why you’re experiencing certain symptoms and develop an appropriate management plan. This could range from simple dietary adjustments to further diagnostic testing or even medication. Remember that the vast majority of people adjust well to life without a gallbladder, so proactive monitoring is about ensuring you’re one of them. A helpful strategy may be weekend recovery meals that reset digestion after overeating.
Diagnostic Tests for Post-Cholecystectomy Issues
When symptoms persist beyond the expected recovery period, your doctor may recommend several tests to evaluate digestive function and rule out other potential causes. One common test is a stool analysis, which can help identify malabsorption issues or infections. This involves collecting stool samples over a specified period (usually 3 days) and sending them to a laboratory for analysis. The results can reveal information about fat absorption, the presence of bile acids, and any signs of inflammation. Another valuable tool is an HIDA scan (hepatobiliary iminodiacetic acid scan), which assesses bile flow from the liver to the small intestine. This involves intravenous injection of a radioactive tracer that allows doctors to visualize the biliary system and identify any blockages or abnormalities in bile drainage.
Beyond these, blood tests play a vital role. Liver function tests (LFTs) are often repeated post-surgery to ensure there’s no damage to the liver itself. Elevated LFTs could indicate complications like bile duct injury or inflammation. Additionally, tests measuring amylase and lipase levels can help rule out pancreatitis, which can sometimes occur as a complication of gallbladder surgery. Depending on your symptoms, your doctor might also consider more specialized tests like a breath test to assess carbohydrate malabsorption, or an endoscopy/colonoscopy to evaluate the digestive tract for other potential issues. It’s crucial to understand that these tests aren’t meant to scare you; they’re simply tools to provide a clearer picture of what’s happening inside your body and guide treatment decisions.
Addressing Bile Acid Malabsorption
Bile acid malabsorption (BAM) is one of the most common causes of chronic diarrhea after gallbladder removal. Because the gallbladder isn’t there to concentrate bile, it can lead to excessive amounts entering the colon, causing irritation and resulting in frequent bowel movements. Diagnosing BAM typically involves a 7α-hydroxy bile acid breath test (also known as a Bile Acid Malabsorption Test or BAM test). This non-invasive test measures the amount of bile acids absorbed in the small intestine; low absorption levels suggest BAM. – The patient ingests a capsule containing a radioactive substance that reacts with bile acids. – Breath samples are collected over several hours. – The concentration of the radioactive substance in the breath indicates how well bile acids are being absorbed. Simple tea rituals can offer some relief during this process.
If BAM is diagnosed, treatment usually involves bile acid sequestrants. These medications bind to bile acids in the intestine, preventing them from causing diarrhea. Cholestyramine, colestipol, and colesevelam are examples of these drugs. It’s important to note that these medications can sometimes interfere with the absorption of other medications, so your doctor will need to assess potential drug interactions. Dietary changes also play a role in managing BAM symptoms; reducing fat intake can help minimize bile flow and lessen diarrhea.
Investigating Sphincter of Oddi Dysfunction
The Sphincter of Oddi is a muscular valve that controls the flow of bile and pancreatic juices into the small intestine. Dysfunction of this sphincter, known as SOD, can cause abdominal pain, nausea, and vomiting after cholecystectomy. Diagnosing SOD is challenging and often requires specialized testing like manometry – a procedure where pressure measurements are taken within the biliary and pancreatic ducts using a catheter. – Manometry involves inserting a thin, flexible tube through the endoscope into the Sphincter of Oddi. – Pressure readings help determine if the sphincter is functioning properly.
SOD can be classified as Type I (biliary), Type II (pancreatic), or Type III (mixed). Treatment depends on the type and severity of dysfunction and may include endoscopic sphincterotomy – a procedure to widen the sphincter using an endoscope – or medications to relax the sphincter muscles. This is generally reserved for cases where other causes have been ruled out, and symptoms are significantly impacting quality of life.
Ruling Out Other Potential Issues
It’s crucial to remember that digestive symptoms after gallbladder removal can sometimes be caused by conditions unrelated to the surgery itself. Conditions like irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), or celiac disease can mimic post-cholecystectomy syndrome, making accurate diagnosis essential. – Blood tests for markers of inflammation (like CRP and ESR) can help assess for IBD. – Stool tests can rule out infections and identify signs of malabsorption. – Endoscopy/Colonoscopy may be necessary to visually inspect the digestive tract and obtain biopsies if needed.
If these tests reveal an alternative diagnosis, treatment will focus on managing that specific condition rather than solely addressing post-cholecystectomy symptoms. Your doctor might recommend dietary changes, medications, or other therapies tailored to your individual needs. The key takeaway is that a thorough evaluation is essential to ensure you receive the most appropriate care and achieve optimal digestive health after gallbladder removal. You may also find comfort meals helpful during this time. Additionally, understanding pancreatic function can help you better manage your recovery. Finally, consider recovery meals to aid in healing.