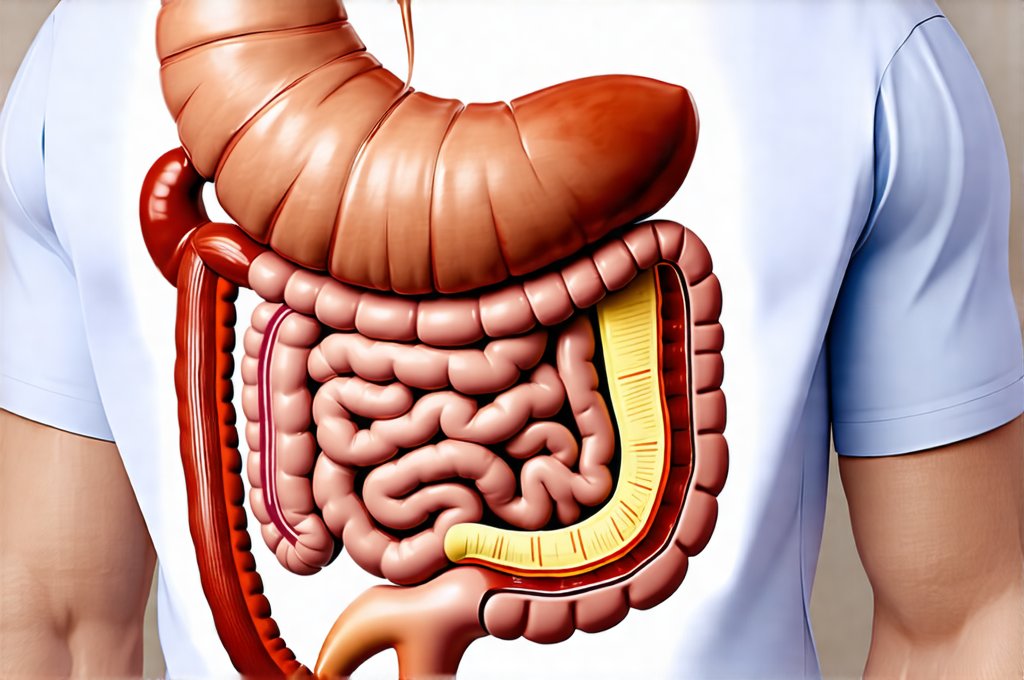
Major life stressors – be they sudden traumatic events like accidents or loss, or prolonged periods of high strain such as job changes, relationship difficulties, or chronic illness in a loved one – can profoundly impact our physical wellbeing. While the immediate emotional fallout often takes center stage, the ripple effects on our digestive system are frequently overlooked. The gut-brain axis, a bidirectional communication network linking these two vital systems, is highly sensitive to stress. When we experience significant stress, hormonal changes, altered motility, and shifts in the gut microbiome can all disrupt normal digestive function, leading to a constellation of symptoms ranging from mild discomfort to debilitating illness. Recognizing this connection is crucial for holistic healing, and often requires moving beyond symptom management to investigate underlying imbalances through appropriate testing. Many individuals find that addressing these post-stress digestive issues isn’t just about alleviating physical suffering; it’s about regaining a sense of control and wellbeing after a challenging time.
The gut is remarkably resilient, but its capacity can be overwhelmed by intense or prolonged stress. This disruption manifests differently in each person, making diagnosis tricky without thorough investigation. Common symptoms include bloating, gas, constipation, diarrhea, abdominal pain, nausea, heartburn, and changes in appetite. However, the impact isn’t limited to these obvious complaints; stress can also exacerbate existing digestive conditions like Irritable Bowel Syndrome (IBS) or Inflammatory Bowel Disease (IBD). Furthermore, it can compromise nutrient absorption, weaken immune function (a significant portion of which resides in the gut), and even contribute to mental health challenges – creating a vicious cycle. Therefore, proactively assessing digestive health after a major stress event isn’t merely about identifying problems; it’s about understanding how stress specifically impacted an individual’s system and tailoring interventions accordingly. Consider looking at comfort meals to help with easing tension during stressful periods.
Understanding the Rationale for Digestive Testing
Digestive testing post-major stress is not a one-size-fits-all recommendation, but rather a thoughtful response to the potential disruptions caused by these events. Often, initial attempts at self-management – dietary changes, increased hydration, stress reduction techniques – are helpful, but they may only address surface symptoms. Testing provides deeper insight into what’s happening beneath the surface, helping to pinpoint specific imbalances that might be contributing to ongoing issues. This level of understanding is invaluable for creating a targeted and effective recovery plan. It moves beyond guesswork and empowers individuals to take informed control of their health journey. If you’ve recently experienced this, daily eating maps can provide structure during difficult times.
A key consideration is the individualized nature of stress responses. What one person experiences as mild discomfort, another may perceive as debilitating pain. Similarly, the physiological impact will vary based on pre-existing conditions, genetic predispositions, coping mechanisms, and the type/duration of the stressor itself. Testing helps to unravel these complexities and identify the unique challenges faced by each individual. It also differentiates between stress-induced digestive issues and other potential underlying causes, ensuring accurate diagnosis and appropriate treatment.
Finally, post-stress digestive problems often don’t resolve spontaneously. Without addressing the root cause – imbalances in gut flora, enzyme deficiencies, intestinal permeability, or inflammation – symptoms may persist for months or even years, significantly impacting quality of life. Testing provides a roadmap for targeted interventions, such as dietary modifications, supplementation, probiotics, or stress management techniques, to restore digestive balance and promote long-term health. Restorative meal ideas can be particularly helpful during the recovery phase.
Common Digestive Tests & Their Applications
When considering digestive testing, it’s important to understand the options available and what each test can reveal. The selection of tests should be guided by an individual’s specific symptoms and medical history, ideally in consultation with a healthcare professional experienced in functional medicine or gut health. Here are some commonly used options:
-
Stool Testing: This is often the first line of investigation. Comprehensive stool analysis (CSA) can assess several key areas:
- Microbiome Analysis: Identifies the diversity and abundance of bacteria, fungi, and other microorganisms in the gut. Imbalances (dysbiosis) are common after stress events.
- Markers of Inflammation: Detects levels of calprotectin or lactoferrin, indicating inflammation in the digestive tract.
- Digestive Enzyme Function: Evaluates pancreatic elastase, a marker of pancreatic function and enzyme sufficiency. Stress can impair digestion.
- Parasites & Pathogens: Identifies potential infections that might be contributing to symptoms.
- Short Chain Fatty Acids (SCFAs): Measures the production of beneficial metabolites by gut bacteria, indicating overall gut health.
-
Small Intestinal Bacterial Overgrowth (SIBO) Testing: SIBO is a condition where excessive bacteria reside in the small intestine, leading to fermentation and digestive symptoms. Breath tests are commonly used to diagnose SIBO, measuring hydrogen and methane levels after consuming a specific sugar solution. Stress can increase intestinal permeability, making individuals more susceptible to SIBO.
-
Food Sensitivity Testing: While controversial, food sensitivity testing (typically IgG or IgA antibody testing) may identify foods that trigger immune responses and contribute to digestive symptoms. It’s important to note these are not the same as food allergies. Stress can alter immune function and potentially exacerbate food sensitivities. This type of testing should be interpreted cautiously and often requires an elimination diet to confirm findings.
Intestinal Permeability (“Leaky Gut”) Assessment
“Leaky gut,” or increased intestinal permeability, is a frequent consequence of chronic stress. The lining of the intestine acts as a barrier, controlling what passes into the bloodstream. When this barrier becomes compromised, larger molecules – undigested food particles, bacteria, toxins – can leak through, triggering immune activation and systemic inflammation. This contributes to a wide range of health problems beyond just digestive symptoms.
Several tests are available to assess intestinal permeability:
– Lactulose/Mannitol Test: Considered the gold standard, this test involves consuming lactulose and mannitol (sugars) and measuring their excretion in urine. Lactulose is poorly absorbed and should remain largely in the gut; increased urinary excretion suggests a leaky gut. Mannitol, conversely, is readily absorbed, so its levels indicate absorption rate.
– Zonulin Levels: Zonulin is a protein that regulates intestinal permeability. Elevated zonulin levels in stool or blood suggest increased leakiness. However, testing for zonulin is still relatively new and the clinical utility remains debated.
Addressing intestinal permeability involves repairing the gut lining through dietary changes (reducing inflammatory foods, incorporating healing nutrients), supplementation (L-glutamine, zinc, collagen), stress management techniques, and optimizing gut microbiome health. It’s a foundational step in restoring digestive function and overall wellbeing post-stress. Warm grain recipes can be very soothing during this process.
The Importance of Personalized Interpretation & Follow-Up
It’s critical to remember that test results are just one piece of the puzzle. They must be interpreted within the context of an individual’s complete health history, symptoms, lifestyle factors, and stress experiences. Self-diagnosis based solely on testing is strongly discouraged. Working with a qualified healthcare professional – a functional medicine practitioner, gastroenterologist specializing in gut health, or registered dietitian – ensures accurate interpretation and development of a personalized treatment plan. Filling grain bowls offer a gentle way to reintroduce foods as you heal.
Following up with repeat testing may also be necessary to monitor progress and adjust interventions as needed. Digestive health is dynamic, and the healing process takes time. Regular assessment helps to ensure that the chosen strategies are effective and that any new imbalances are addressed promptly. Ultimately, digestive testing after major stress events is an investment in long-term health and wellbeing, empowering individuals to regain control of their bodies and lives. It’s about moving beyond merely coping with symptoms to understanding the underlying causes and restoring a healthy gut-brain connection. If you’re feeling overwhelmed during this time, remember to consider how to reduce digestive stress after stressful events.