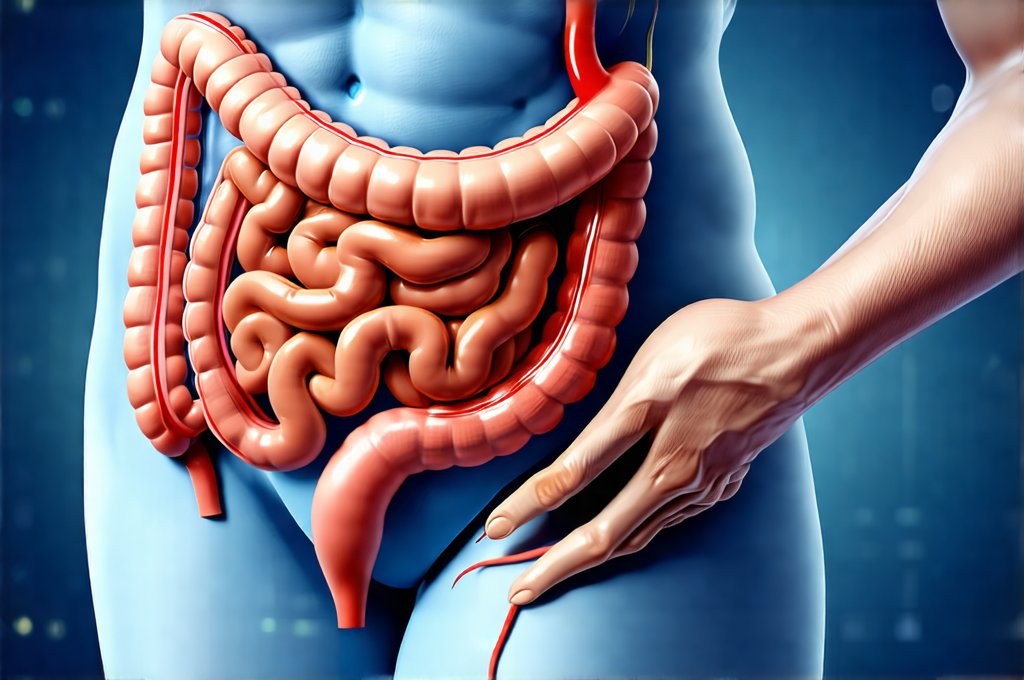
Recurring gut pressure and discomfort are surprisingly common experiences, impacting millions worldwide. Often dismissed as ‘just stress’ or attributed to dietary indiscretions, persistent symptoms can significantly diminish quality of life, affecting everything from sleep and energy levels to mental wellbeing and social activities. The complexity stems partly from the gut’s intimate connection with other body systems – it’s not simply a digestive tract but a central player in immunity, mood regulation, and even neurological function. Understanding this intricate interplay is crucial for navigating these challenges effectively, moving beyond quick fixes towards lasting solutions that address root causes rather than just masking symptoms.
The traditional approach to gut issues often focused on identifying specific pathologies – ulcers, inflammatory bowel disease (IBD), etc. While vital for diagnosing serious conditions, it frequently overlooked the vast number of individuals experiencing chronic, less defined discomfort without a clear-cut diagnosis. This has led to a rise in functional gastrointestinal disorders (FGIDs) like Irritable Bowel Syndrome (IBS), where symptoms are real and debilitating but conventional tests yield normal results. Modern approaches acknowledge this grey area, shifting towards holistic assessments that consider the multifaceted nature of gut health and personalized interventions tailored to individual needs. This article will explore these evolving strategies for managing recurring gut pressure and discomfort, focusing on lifestyle adjustments, dietary modifications, and emerging therapeutic options.
Understanding the Root Causes
The sensation of “gut pressure” can stem from a multitude of factors, rarely being attributable to one single cause. It’s often a combination of physiological, psychological, and lifestyle elements working in concert. One key area is visceral hypersensitivity – an increased sensitivity to normal gut activity. What feels like mild stretching or gas production to one person might register as intense pressure or pain for another. This isn’t necessarily a sign of disease but rather a heightened awareness within the nervous system.
Beyond hypersensitivity, mechanical factors play a role. These can include bloating from excessive gas production (often linked to diet), slow gut motility leading to constipation and build-up of waste, or even structural issues like pelvic floor dysfunction. Furthermore, the brain-gut axis – the bidirectional communication pathway between the digestive system and the central nervous system – is profoundly influential. Stress, anxiety, and depression can directly impact gut function, exacerbating symptoms and creating a vicious cycle. Chronic stress alters gut motility, increases inflammation, and even changes the composition of the gut microbiome. Understanding gut transit time can be crucial in identifying underlying causes.
Finally, dietary factors are consistently implicated. Food intolerances (distinct from allergies), sensitivities to specific carbohydrates (like FODMAPs – Fermentable Oligosaccharides, Disaccharides, Monosaccharides And Polyols), and poor dietary habits can all contribute to discomfort. Identifying these triggers often requires careful self-monitoring or guided elimination diets. It’s vital to remember that gut health is incredibly individual; what works for one person may not work for another. Considering food rituals can also help improve the digestive process.
Dietary Strategies for Gut Comfort
Diet plays a monumental role in managing gut pressure and discomfort, but it’s rarely about strict restriction. Instead, the focus should be on optimizing dietary patterns to support healthy digestion and reduce inflammation. A cornerstone of many modern approaches is the Low-FODMAP diet, developed by researchers at Monash University. This isn’t intended as a long-term solution but rather a diagnostic tool to identify trigger foods. It involves temporarily eliminating high-FODMAP foods – things like onions, garlic, apples, wheat, and certain dairy products – then systematically reintroducing them to determine individual sensitivities.
- Step 1: Elimination Phase (2-6 weeks) – Strictly avoid all high-FODMAP foods
- Step 2: Reintroduction Phase – Gradually introduce one FODMAP group at a time, monitoring symptoms closely.
- Step 3: Personalization Phase – Build a long-term diet based on tolerated foods, incorporating variety and nutritional balance.
Beyond FODMAPs, prioritizing whole, unprocessed foods is crucial. Emphasize lean proteins, healthy fats (like omega-3 fatty acids), fiber-rich vegetables, and fruits with lower fructose content. Hydration is also key; adequate water intake supports regular bowel movements and prevents constipation. Consider incorporating prebiotic foods – those that feed beneficial gut bacteria – like asparagus, bananas, and oats in tolerated amounts. A registered dietitian specializing in gut health can provide personalized guidance and ensure nutritional adequacy during dietary changes. Focusing on gut health simple strategies makes long term adherence easier.
The Role of the Gut Microbiome
The gut microbiome – the trillions of microorganisms residing in our digestive tract – is increasingly recognized as a central player in overall health, including gut comfort. An imbalance in these microbial communities (known as dysbiosis) can contribute to inflammation, altered motility, and increased visceral sensitivity. Factors like antibiotic use, stress, poor diet, and chronic illness can disrupt the microbiome’s delicate balance.
Restoring a healthy microbiome is often a key component of modern gut health strategies. This can be achieved through several avenues: dietary interventions (emphasizing fiber-rich foods), probiotic supplementation (introducing beneficial bacteria), and even fecal microbiota transplantation (FMT) in specific cases under medical supervision. Probiotics are available in various strains, each potentially offering different benefits. Choosing the right strain for your specific needs requires careful consideration – a healthcare professional can help guide selection. However, it’s important to note that probiotics aren’t a universal fix; their effectiveness varies considerably between individuals. Gut inflammation can also significantly impact microbiome health.
Stress Management and Mind-Body Techniques
Given the strong connection between the brain and gut, managing stress is paramount in alleviating recurring discomfort. Chronic stress elevates cortisol levels, which can disrupt gut motility, increase inflammation, and negatively impact the microbiome. Integrating stress management techniques into daily life is therefore essential.
Techniques like mindfulness meditation, deep breathing exercises, yoga, and regular physical activity have all demonstrated benefits for reducing stress and improving gut function. Cognitive Behavioral Therapy (CBT) specifically tailored to gut health issues can also be highly effective. CBT helps individuals identify and modify negative thought patterns and behaviors that exacerbate symptoms. Biofeedback – a technique that teaches you to control physiological responses like heart rate and muscle tension – may also prove beneficial for some. Prioritizing self-care, setting boundaries, and building strong social support networks are all crucial aspects of stress management. Addressing gut transit and related discomforts can also help reduce overall stress levels. When dealing with children, it’s important to understand child’s gut trouble. For infants experiencing discomfort, there are gentle ways to ease gas and belly pressure.
It’s essential to consult with a healthcare professional before making significant changes to your diet or starting any new supplements or therapies. This information is for general knowledge and informational purposes only, and does not constitute medical advice. It is always best to seek the advice of a qualified healthcare provider for any questions you may have regarding your health or treatment.