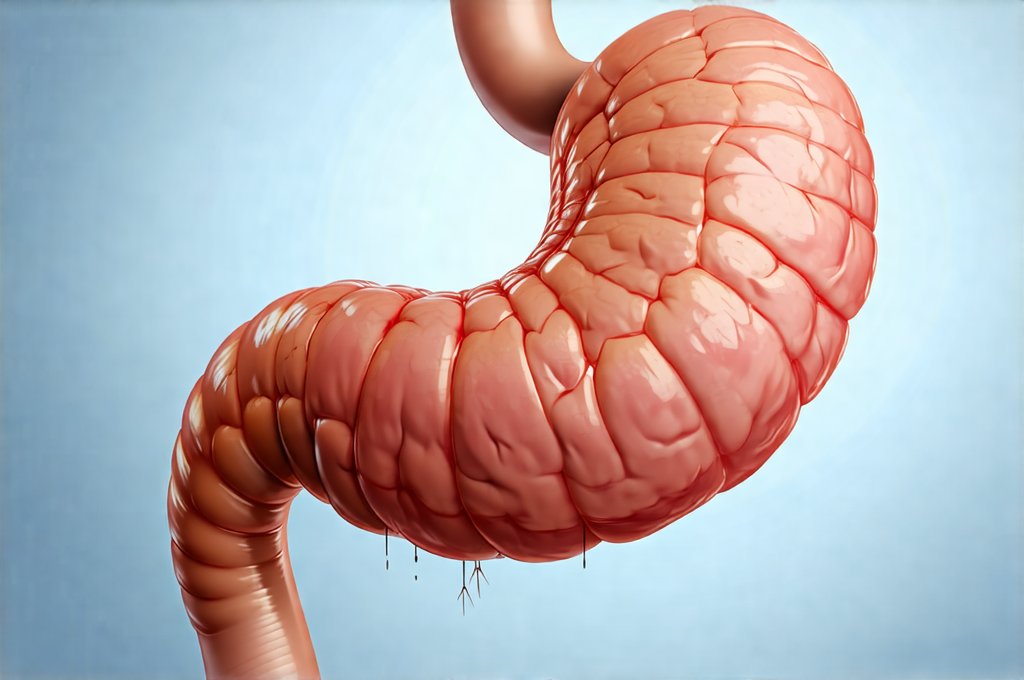
Our digestive systems are remarkable machines, constantly working to break down food, absorb nutrients, and eliminate waste. We often focus on what we eat, but rarely consider how we eat – and the seemingly innocuous act of swallowing air can profoundly impact this process. Air swallowing, or aerophagia as it’s formally known, is a surprisingly common phenomenon that many people experience without even realizing it. It’s not usually cause for alarm, but excessive air swallowing can lead to uncomfortable symptoms like bloating, belching, abdominal discomfort, and even disrupt normal digestive function. Understanding the mechanics of this process and identifying potential contributing factors are key to managing its effects and promoting overall gut health.
This article will delve into the relationship between air swallowing and digestive health, exploring how it happens, why it might become problematic, and what steps can be taken to minimize its impact. We’ll examine both physiological causes and behavioral patterns that contribute to excessive aerophagia, as well as strategies for mitigating symptoms and supporting a healthier digestive experience. It’s important to remember that while this information is intended to be informative, it should not replace the advice of a qualified healthcare professional; if you have persistent or severe digestive issues, seeking medical evaluation is crucial.
The Mechanics of Aerophagia & Digestive Disruption
Air swallowing isn’t inherently bad – we all do it to some extent. It happens during normal eating and drinking, as well as during everyday activities like talking and breathing. However, the problem arises when excessive amounts of air are swallowed, or when that air isn’t adequately released through belching. This excess gas can then accumulate in the digestive tract, leading to a variety of unpleasant symptoms. The digestive system is designed to process food efficiently, but introducing excessive air disrupts this process, potentially altering motility – the movement of food through the gut.
- Increased pressure within the digestive tract from trapped air can lead to feelings of bloating and fullness.
- This pressure can also affect the function of the lower esophageal sphincter (LES), which prevents stomach acid from flowing back into the esophagus, potentially exacerbating symptoms of heartburn or acid reflux.
- The presence of excess gas can interfere with nutrient absorption as it physically alters the digestive environment.
The amount of air we swallow varies considerably depending on individual habits and underlying conditions. Some people are naturally more prone to aerophagia than others due to differences in swallowing patterns or anatomical factors. Furthermore, certain behaviors – such as eating quickly, chewing gum, smoking, drinking carbonated beverages, or even wearing ill-fitting dentures – can significantly increase the amount of air ingested. The digestive system has a limited capacity for handling excess gas and when overwhelmed, symptoms begin to appear. Understanding gut health is crucial here.
Common Causes & Contributing Factors
Identifying the root causes of excessive aerophagia is essential for effective management. While some individuals develop habitual swallowing patterns that lead to increased air intake, others may experience it as a secondary symptom related to underlying medical conditions or lifestyle choices. One common contributor is rapid eating. When we eat quickly, we tend to gulp down food along with more air, giving our digestive system less time to process everything efficiently. Similarly, chewing gum forces us to constantly swallow, increasing the amount of air taken in.
Beyond behavioral factors, certain medical conditions can also contribute to aerophagia. Gastroesophageal reflux disease (GERD), for example, can sometimes lead to increased swallowing as individuals attempt to clear acid from their esophagus. Anxiety and stress are also significant factors; when stressed, people often unconsciously swallow more air, and this can create a vicious cycle where digestive discomfort exacerbates anxiety levels. Finally, certain medications or medical conditions affecting esophageal motility – like achalasia – may disrupt normal swallowing patterns and contribute to aerophagia. It’s important to note that pinpointing the exact cause often requires careful observation of individual habits and potentially consultation with a healthcare professional. The link between gut immunity can also play a role here.
Lifestyle Adjustments for Reducing Air Swallowing
Fortunately, many cases of mild to moderate aerophagia can be effectively managed through simple lifestyle adjustments. These changes focus on modifying behaviors that contribute to excessive air intake and promoting more mindful eating habits.
- Slow down your eating: Consciously slowing down the pace of meals allows for better chewing and reduces the amount of air swallowed with each bite. Aim to take smaller bites and savor each mouthful.
- Avoid carbonated beverages: These drinks are inherently filled with gas, which contributes directly to bloating and discomfort. Opt for water, herbal teas, or other non-carbonated alternatives.
- Limit chewing gum & hard candies: Prolonged chewing encourages air swallowing, while sucking on hard candies can have a similar effect.
- Manage stress levels: Incorporate stress-reducing techniques such as meditation, yoga, deep breathing exercises, or spending time in nature.
These adjustments may seem small, but their cumulative effect can be significant in reducing the amount of air ingested and easing digestive discomfort. It’s about creating a more mindful approach to eating and being aware of habits that might unintentionally contribute to aerophagia. Regular daily walks could also help.
Dietary Considerations & Food Sensitivities
While lifestyle changes are often the first line of defense, dietary modifications can also play a supportive role in managing aerophagia. Certain foods are known to produce more gas during digestion – such as beans, broccoli, cabbage, and onions – and reducing intake of these fermentable carbohydrates (FODMAPs) may alleviate symptoms for some individuals. However, it’s important to avoid unnecessarily restrictive diets without proper guidance from a healthcare professional or registered dietitian.
- Identify potential food sensitivities: Food intolerances can sometimes contribute to digestive distress and indirectly exacerbate aerophagia. Keeping a food diary and tracking symptoms can help identify trigger foods.
- Consider probiotics: While more research is needed, some studies suggest that probiotics – beneficial bacteria found in fermented foods or supplements – may improve gut health and reduce gas production.
- Stay hydrated: Drinking plenty of water helps maintain healthy digestion and can prevent constipation, which can worsen bloating and discomfort.
It’s crucial to remember that dietary needs vary significantly from person to person. What works for one individual might not work for another, so it’s essential to experiment cautiously and seek professional guidance when necessary. Gut is healing with the right diet.
When to Seek Medical Attention
While most cases of aerophagia are mild and manageable with lifestyle adjustments, there are instances where medical evaluation is warranted. If symptoms are severe, persistent, or significantly interfere with daily life, it’s important to consult a healthcare professional. Red flag symptoms include:
- Severe abdominal pain
- Persistent nausea or vomiting
- Unintentional weight loss
- Difficulty swallowing (dysphagia)
- Changes in bowel habits
These symptoms could indicate an underlying medical condition that requires diagnosis and treatment. A doctor may recommend diagnostic tests – such as endoscopy, barium swallow studies, or gastric emptying studies – to evaluate the digestive system and identify any abnormalities. They can also help rule out other potential causes of digestive discomfort and develop a personalized management plan tailored to your specific needs. Do not self-diagnose or attempt to treat serious digestive issues without professional medical guidance. If you are traveling, consider how travel affects your digestion too. Are meal replacements bad for your gut?