Gastrointestinal (GI) investigations are crucial for diagnosing a wide range of digestive ailments, from subtle discomforts to life-threatening conditions. Traditionally, colonoscopy and endoscopy have been the gold standard methods for visualizing the GI tract. However, these procedures involve inserting a camera attached to a flexible tube through natural body openings (mouth or rectum), which can be uncomfortable for patients and carries some inherent risks, even if minimal. In recent decades, capsule endoscopy has emerged as a compelling alternative – and sometimes complement – to conventional endoscopic methods. This minimally invasive technique utilizes a tiny, disposable camera that is swallowed by the patient and transmits images of the small intestine as it travels through the digestive system. The question then arises: in what scenarios does capsule endoscopy surpass traditional endoscopy, and where do the strengths of conventional methods remain paramount?
The choice between these two approaches isn’t simply about one being “better” than the other. It’s about selecting the most appropriate tool for a specific diagnostic challenge. Traditional endoscopy excels at allowing intervention – biopsies can be taken, polyps removed, and bleeding stopped directly during the procedure. Capsule endoscopy, on the other hand, focuses primarily on visualization; it’s exceptional at exploring areas inaccessible to standard endoscopes, particularly the small intestine, but lacks immediate interventional capabilities. This article will delve into the nuances of both methods, comparing their strengths, weaknesses, and ideal applications, ultimately aiming to clarify when a capsule endoscopy might be preferable.
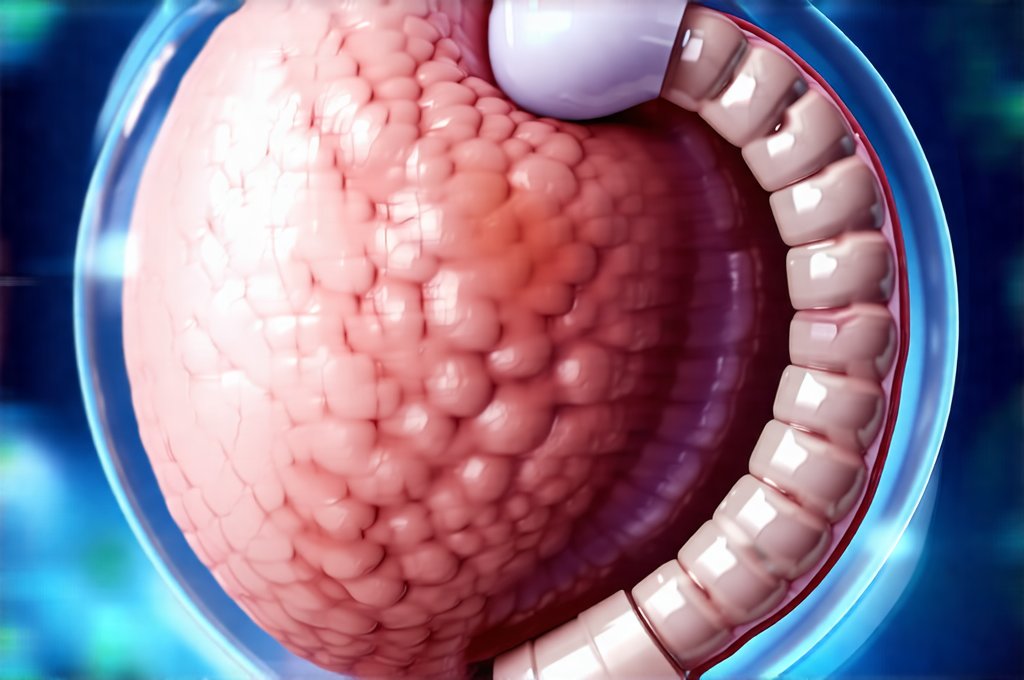
Understanding Traditional Endoscopy & Colonoscopy
Traditional endoscopy encompasses several variations depending on which part of the GI tract is being examined. Upper endoscopy (also known as esophagogastroduodenoscopy or EGD) visualizes the esophagus, stomach, and duodenum – the first part of the small intestine. A flexible endoscope is inserted through the mouth. Colonoscopy, conversely, examines the large intestine (colon) using a similar flexible tube introduced rectally. Both procedures require bowel preparation for colonoscopies and often sedation to ensure patient comfort. The key advantage of traditional endoscopy lies in its ability to both visualize and intervene. This means doctors can take tissue samples (biopsies) for further analysis, remove polyps that could potentially become cancerous, or stop bleeding from ulcers – all during the same procedure.
This interventional capability makes traditional endoscopy and colonoscopy invaluable in diagnosing and treating a wide spectrum of conditions. For example, if a patient presents with unexplained anemia, a colonoscopy can detect sources of bleeding, like polyps or angiodysplasia. Similarly, upper endoscopy is crucial for investigating symptoms like persistent heartburn, abdominal pain, or difficulty swallowing. The procedure provides immediate feedback; abnormalities are identified and addressed in real-time. However, the preparation process – especially for colonoscopies – can be unpleasant, and there’s a small risk of perforation (a tear in the intestinal wall) associated with inserting the endoscope.
The small intestine, however, poses a significant challenge to traditional endoscopy. While specialized enteroscopes exist, they are often difficult to navigate through the entire length of the small bowel, leaving substantial portions unexplored. This is where capsule endoscopy truly shines. It bypasses many of these limitations by offering a non-invasive way to visualize the entire small intestine – an area traditionally hard to reach and frequently overlooked in GI investigations. If you experience frequent gas, it’s important to how to tell if your gas is a sign of something more serious.
The Rise of Capsule Endoscopy: A Different Approach
Capsule endoscopy represents a paradigm shift in how we examine the small intestine. A patient simply swallows a tiny capsule, roughly the size of a vitamin pill, containing a camera, light source, battery, and transmitter. As it travels through the digestive system (a process taking approximately 8-12 hours), the capsule transmits images wirelessly to a recorder worn by the patient. This procedure is significantly less invasive than traditional endoscopy, requiring minimal preparation beyond avoiding solid food for a short period beforehand. Patients can generally resume their normal activities during the recording phase, although there may be some restrictions on strenuous exercise.
The real strength of capsule endoscopy lies in its ability to provide comprehensive visualization of the small intestine – something conventional endoscopes struggle with. This is particularly useful in diagnosing conditions like Crohn’s disease, where inflammation can occur throughout the GI tract, including the small bowel. It’s also excellent for identifying sources of bleeding that are difficult to locate with colonoscopy or upper endoscopy. While it cannot take biopsies or perform interventions directly, it can pinpoint areas requiring further investigation – often leading to targeted procedures. When considering dietary choices, you may wonder is there a safe way to enjoy chocolate with GERD?
However, capsule endoscopy isn’t without its limitations. The disposable nature of the capsules makes them relatively expensive, though costs have been decreasing over time. Image quality can sometimes be affected by food residue or rapid transit through the bowel. Importantly, if an abnormality is detected, a follow-up colonoscopy or upper endoscopy is usually needed to obtain biopsies and potentially treat the condition. The impact of gut health plays a bigger role in reflux than we think should also be considered.
Diagnosing Obscure GI Bleeding
One of the most common applications of capsule endoscopy is in the investigation of obscure GI bleeding. This refers to bleeding from the digestive tract that cannot be identified by standard endoscopy (upper and/or colonoscopy). Often, this originates in the small intestine – a region challenging for traditional techniques. Capsule endoscopy excels here because it provides a complete view of the entire small bowel, allowing doctors to pinpoint the source of bleeding with greater accuracy.
- The process typically involves a preparation period focusing on clear liquid diet and potentially certain laxatives to ensure optimal visualization.
- During the capsule ingestion, the patient wears a recorder that captures images from the capsule as it travels through the digestive system.
- After the recording is complete (usually within 12 hours), the data is downloaded and analyzed by a gastroenterologist.
If a source of bleeding is identified, further intervention may be necessary. This might involve colonoscopy or upper endoscopy to obtain biopsies or stop the bleeding using techniques like cauterization. Capsule endoscopy doesn’t stop the bleeding itself, but it dramatically improves the chances of finding the origin and guiding subsequent treatment. This targeted approach significantly reduces the need for unnecessary investigations. It is important to rule out is it acid reflux or a sign of something more serious?
Identifying Small Bowel Crohn’s Disease
Crohn’s disease, a chronic inflammatory bowel disease, can affect any part of the digestive tract, including the small intestine. Traditional endoscopy often struggles to reach all areas of the small bowel, making diagnosis challenging. Capsule endoscopy provides a more comprehensive view, allowing doctors to identify inflammation, ulcers, and other signs of Crohn’s disease in the small intestine.
- The high resolution images captured by the capsule can reveal subtle changes indicative of early-stage disease that might be missed by conventional methods.
- This is particularly valuable for patients with atypical symptoms or those who have had negative results from previous endoscopic examinations.
- While capsule endoscopy cannot confirm Crohn’s disease definitively (biopsies are still required), it helps to narrow down the location and extent of inflammation, guiding further diagnostic steps.
The ability to visualize the entire small intestine is especially important in cases where Crohn’s disease affects multiple segments or has an atypical presentation. It allows for a more accurate assessment of disease activity and can influence treatment decisions.
Assessing Other Small Intestinal Disorders
Beyond bleeding and Crohn’s disease, capsule endoscopy proves useful in diagnosing a variety of other small intestinal disorders. These include:
- Celiac Disease: Though often diagnosed through blood tests, capsule endoscopy can assess the extent of damage to the small intestinal lining caused by gluten intolerance.
- Small Intestinal Tumors: While rare, tumors in the small intestine can be difficult to detect with traditional methods. Capsule endoscopy provides a non-invasive way to screen for these abnormalities.
- Meckel’s Diverticulum: A congenital abnormality where a pouch forms on the small intestine; capsule endoscopy can help identify this and associated complications.
- Lymphoma: Small intestinal lymphoma can be diagnosed through analysis of images captured by the capsule, although biopsy confirmation is still needed.
In each of these scenarios, the ability to visualize the entire small intestine without invasive procedures makes capsule endoscopy a valuable diagnostic tool. It’s important to remember that it often serves as a first step in the diagnostic process, followed by more targeted investigations if necessary. The importance of digestive enzymes work better than others should not be overlooked when considering overall gut health.
Ultimately, the “better” method isn’t about declaring one superior overall; it is about choosing the most appropriate tool for the specific clinical scenario and patient needs. Both capsule endoscopy and traditional endoscopy play vital roles in gastrointestinal diagnostics, often complementing each other to provide a comprehensive understanding of digestive health. Also consider sitting in a reclined position is bad after meals and its impact on digestion.