Antacids are readily available over-the-counter remedies often used to quickly neutralize stomach acid, providing temporary relief from heartburn, indigestion, and upset stomachs. They’ve become incredibly common in modern life, viewed by many as a harmless fix for occasional digestive discomfort. However, while they can offer immediate symptomatic relief, frequent or long-term reliance on antacids – even seemingly mild ones – can significantly disrupt the delicate ecosystem within your gut, leading to a cascade of unintended consequences that extend far beyond just temporary relief. Understanding how your gut reacts to overuse is crucial for making informed decisions about digestive health and avoiding potential problems down the line.
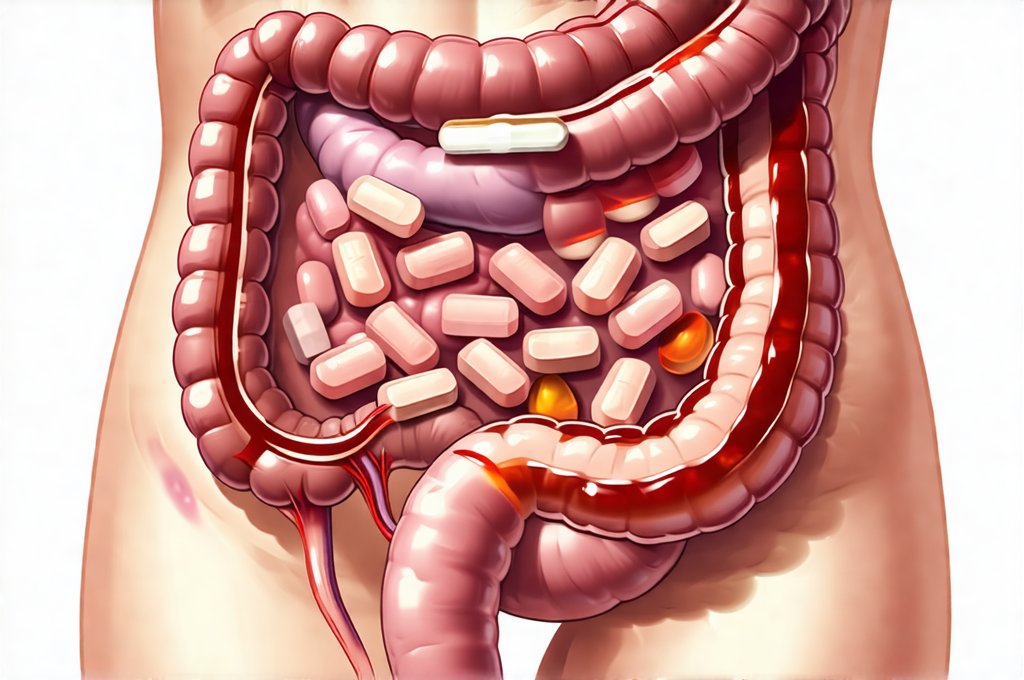
The human digestive system is an intricate network designed for optimal function, relying on a precise balance of acidity, enzymes, and beneficial bacteria. Antacids, by design, interfere with this natural process. While addressing symptoms like heartburn can feel necessary, consistently suppressing stomach acid doesn’t address the root cause of the issue – it merely masks it. This prolonged interference can alter gut flora composition, impair nutrient absorption, and potentially exacerbate underlying digestive conditions. It’s important to remember that stomach acid isn’t the enemy; it plays a vital role in breaking down food, sterilizing ingested materials, and initiating protein digestion. If you are struggling with reflux medication, consider rebuild gut health.
The Impact on Gut Microbiome Diversity
The gut microbiome – the vast community of bacteria, fungi, viruses, and other microorganisms residing in your digestive tract – is increasingly recognized as a cornerstone of overall health. These microbes perform essential functions, including aiding in digestion, synthesizing vitamins, modulating immunity, and even influencing mood. Overuse of antacids disrupts this delicate balance. Antacids elevate the pH level within the stomach and intestines, creating an environment less favorable to beneficial bacteria while potentially allowing harmful ones to proliferate. This shift in microbial composition is called dysbiosis.
Dysbiosis isn’t simply about having “bad” bacteria; it’s about losing diversity. A healthy gut boasts a wide range of species working synergistically. Antacid overuse can narrow this diversity, making the gut ecosystem more vulnerable to imbalances and less resilient when faced with challenges like stress or dietary changes. This loss of microbial richness has been linked to several health concerns beyond digestive issues, including immune dysfunction, increased inflammation, and even mental health conditions. It’s a complex interplay, but reducing acidity too frequently can create an environment where beneficial microbes struggle to thrive, allowing less desirable species to dominate. If you are concerned about imbalance, learn early signs.
Furthermore, some antacids contain ingredients like aluminum or magnesium which can directly impact microbial populations. While these metals are often present in small amounts, chronic exposure through frequent antacid use can further contribute to dysbiosis and potentially inhibit the growth of essential gut bacteria. The long-term consequences of this altered microbiome are still being researched, but emerging evidence suggests it’s a significant factor in many chronic health conditions.
Nutrient Absorption Interference
One of the most crucial functions of stomach acid is its role in nutrient absorption. Many vitamins and minerals require an acidic environment to be properly broken down and absorbed by the body. For example, vitamin B12, iron, calcium, zinc, and magnesium all rely on sufficient stomach acidity for optimal uptake. By chronically reducing this acidity, antacids can lead to deficiencies in these essential nutrients – even if you’re consuming a diet rich in them.
- Reduced B12 absorption: Vitamin B12 requires intrinsic factor, produced by cells in the stomach, which only functions effectively in an acidic environment.
- Impaired iron uptake: Iron exists in different forms; the form readily absorbed by the body (ferrous iron) is facilitated by stomach acid.
- Compromised calcium assimilation: Calcium absorption relies on a specific pH range that antacids can disrupt.
This isn’t just about preventing deficiencies. Nutrient malabsorption can lead to fatigue, weakened immunity, bone health issues, and a host of other health problems. It’s important to note that these effects are often subtle and develop over time, making them difficult to recognize without proper testing. The body may initially compensate for reduced absorption, but eventually, deficiencies will manifest as noticeable symptoms. Understanding how your gut is healing can help you monitor progress.
The Acid Rebound Effect
Ironically, long-term antacid use can actually increase acid production in the stomach – a phenomenon known as the “acid rebound effect.” When you consistently suppress acid secretion with medication, your stomach responds by producing more acid to compensate. This creates a vicious cycle where you need increasingly higher doses of antacids to achieve the same level of relief.
The body attempts to maintain homeostasis, and constantly blocking acid production signals it to ramp up its own output. This can lead to even worse heartburn and indigestion symptoms when you try to reduce or stop taking antacids. It’s a challenging situation for many people who become dependent on these medications, finding themselves trapped in a cycle of increasing dosage and worsening symptoms.
Digestive Enzyme Activity & Food Breakdown
Stomach acid isn’t just about dissolving food; it also activates digestive enzymes like pepsin, which are crucial for breaking down proteins. Reducing stomach acidity can impair the function of these enzymes, leading to incomplete protein digestion. Undigested proteins can then ferment in the gut, contributing to bloating, gas, and other digestive discomforts. This maldigestion can also lead to increased intestinal permeability – often referred to as “leaky gut” – where undigested food particles pass into the bloodstream, potentially triggering inflammation and immune responses.
Furthermore, proper digestion is essential for nutrient breakdown. Without adequate enzyme activity, even healthy foods may not be fully utilized by the body. This can exacerbate nutrient deficiencies and contribute to a range of health problems over time. The gut’s ability to efficiently process food relies on this delicate balance between acidity and enzymatic action; antacid overuse disrupts this vital interplay, hindering optimal digestion and absorption. Before you travel, plan ahead with travel tips.
It’s crucial to address the underlying causes of heartburn and indigestion rather than simply masking symptoms with antacids. Lifestyle modifications such as dietary changes (reducing trigger foods like spicy or fatty meals), stress management techniques, weight management, and identifying food sensitivities can often provide more sustainable relief without disrupting gut health. If you’re experiencing frequent digestive discomfort, consulting a healthcare professional is essential to determine the root cause and develop an appropriate treatment plan that prioritizes long-term well-being over temporary symptom suppression. It’s also helpful to talk to family about your needs, so they can support you. Consider how to make your pantry gut friendly for optimal health. And remember that eating out doesn’t have to stress your gut – learn how to eat out.