Reflux, commonly experienced as heartburn, is a frustrating condition affecting millions. While many automatically equate reflux with excess stomach acid, this isn’t always the case. In fact, identifying whether your reflux is acidic or non-acidic can significantly impact how you manage it and what treatments provide relief. Many people self-treat based on the assumption of acidity, potentially missing out on effective strategies for non-acidic reflux which requires a different approach altogether. This article aims to delve into the nuances of both types of reflux, offering insights into recognizing the symptoms and understanding potential underlying causes so you can better navigate this common health concern.
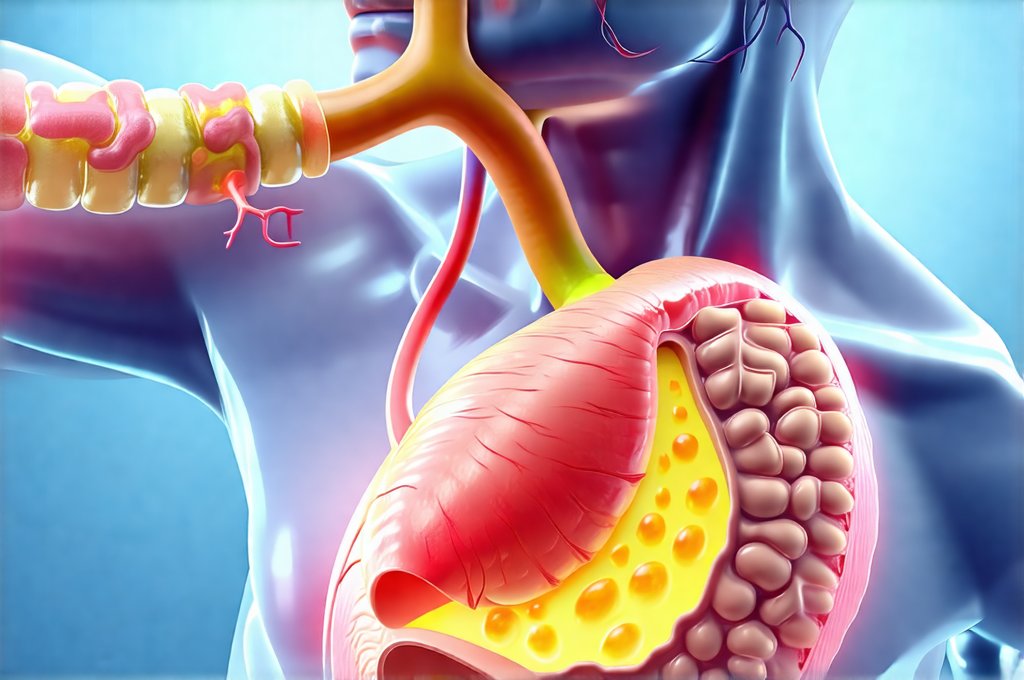
The experience of reflux, regardless of its acidity level, stems from stomach contents flowing back up into the esophagus. The esophagus lacks the protective lining of the stomach, making it vulnerable to irritation. However, the composition of that backflow dictates the nature and severity of symptoms. Acidic reflux is caused by hydrochloric acid (HCl) produced in the stomach, while non-acidic reflux can be triggered by bile salts, enzymes like pepsin, or even just solid food particles. Understanding this fundamental difference is crucial because treatments designed for acidic reflux – such as antacids or proton pump inhibitors – won’t necessarily alleviate symptoms of non-acidic reflux and might even worsen them in some cases.
Recognizing Acidic vs. Non-Acidic Reflux
The classic heartburn sensation – a burning feeling rising from the chest towards the throat – is strongly associated with acidic reflux. However, this isn’t always definitive. While burning is typical for acid reflux, non-acidic reflux often presents differently. Non-acidic reflux sufferers frequently describe symptoms as more of a raw, sore throat, a lump in the throat sensation (globus), chronic cough, or even hoarseness. The discomfort may feel less like burning and more like irritation or inflammation. It’s important to remember that symptom presentation can vary greatly from person to person, making self-diagnosis challenging.
Acidic reflux tends to be exacerbated by acidic foods – citrus fruits, tomatoes, coffee, spicy dishes – and often flares up after eating. Symptoms might also worsen when lying down or bending over due to gravity aiding the backflow. Non-acidic reflux, conversely, may not have a strong correlation with specific food triggers. It’s more likely to be linked to fat-rich meals which stimulate bile release, or large meal sizes that increase pressure in the stomach. The timing of symptoms can also differ; non-acidic reflux often occurs several hours after eating, as the digestive process progresses and bile acids are mobilized.
Finally, a key differentiator lies in response to acid-suppressing medications. If your heartburn significantly improves with antacids or proton pump inhibitors (PPIs), it’s highly likely you’re dealing with acidic reflux. However, if these medications offer little to no relief – or even worsen your symptoms – non-acidic reflux should be strongly considered. This is a critical observation that warrants further investigation and potentially different treatment strategies. It’s vital to note this isn’t a substitute for professional medical diagnosis; it merely provides clues. If you are unsure about reactions, consider how to tell if you’re reacting to spices.
Identifying Potential Causes
Determining the underlying cause of reflux, whether acidic or non-acidic, can guide effective management. Acidic reflux is frequently linked to conditions like gastroesophageal reflux disease (GERD), hiatal hernia, or Helicobacter pylori infection. Lifestyle factors such as obesity, smoking, and a diet high in processed foods can also contribute. These causes generally involve an overproduction of stomach acid or a weakened lower esophageal sphincter (LES) allowing for easier backflow.
Non-acidic reflux, on the other hand, is often associated with postprandial bile reflux (PBR), where bile salts flow back into the esophagus after eating. This can occur after gallbladder removal (cholecystectomy) as the body lacks a reservoir to regulate bile release. Another cause could be duodenogastric reflux, involving pancreatic enzymes and digestive fluids flowing upwards. Interestingly, some individuals with non-acidic reflux may have a perfectly functioning LES but still experience symptoms due to altered digestive processes or sensitivities to these other substances. If you’re concerned about your overall gut health, exploring how to tell if probiotics are working might be beneficial.
Finally, it’s essential to consider that certain medications can also contribute to both types of reflux. For example, some drugs used to treat osteoporosis can weaken the LES, increasing the risk of acidic reflux. Similarly, certain pain relievers may irritate the esophageal lining, exacerbating symptoms regardless of acidity level. A thorough review of your medication list with a healthcare professional is always advisable.
Diagnostic Tools and When To Seek Help
While self-assessment can offer initial clues, accurate diagnosis requires medical evaluation. Your doctor might begin with a detailed history of your symptoms, dietary habits, and any relevant medical conditions. They may also recommend lifestyle modifications as a first step. However, if symptoms persist or are severe, further testing is often necessary.
One common diagnostic tool is endoscopy, where a thin, flexible tube with a camera is inserted into the esophagus to visually inspect the lining for inflammation or damage. Biopsies can be taken during endoscopy to identify any abnormalities. Another test is esophageal pH monitoring which measures the acidity levels in your esophagus over a period of 24 hours. This helps determine if reflux episodes are primarily acidic. However, standard pH monitoring doesn’t detect non-acidic reflux effectively.
More advanced testing, like impedance-pH monitoring, can detect both acidic and non-acidic reflux by measuring the electrical resistance (impedance) along with pH levels. This provides a more comprehensive picture of what’s flowing back into your esophagus. It’s crucial to seek medical attention if you experience: – Difficulty swallowing – Persistent sore throat that doesn’t improve with over-the-counter remedies – Unexplained weight loss – Chest pain, especially if accompanied by shortness of breath or dizziness – Vomiting blood or having black, tarry stools These symptoms could indicate a more serious underlying condition requiring immediate medical intervention. It might also be worth investigating if you need a gut detox if your symptoms are severe and persistent.
Managing Reflux: A Tailored Approach
The treatment for reflux depends heavily on whether it’s acidic or non-acidic. For acidic reflux, treatments typically focus on reducing stomach acid production. This includes lifestyle changes like avoiding trigger foods, elevating the head of your bed, and losing weight if overweight. Medications such as antacids, H2 blockers, and PPIs are often prescribed to neutralize or reduce acid secretion.
For non-acidic reflux, however, these treatments can be ineffective or even counterproductive. Instead, management focuses on strategies like: – Reducing fat intake, especially after gallbladder removal – Eating smaller, more frequent meals to avoid overfilling the stomach – Avoiding late-night eating – Considering medications that bind bile acids, such as ursodeoxycholic acid (UDCA), though this is often prescribed for specific conditions and under medical supervision.
Ultimately, a personalized approach guided by a healthcare professional is essential. There’s no one-size-fits-all solution to reflux. Accurate diagnosis, coupled with tailored lifestyle modifications and appropriate medication, can significantly improve your quality of life and alleviate the discomfort associated with this common condition. Remember that self-treating without proper evaluation may mask underlying issues or lead to ineffective therapies. How to build trust with your body again is important during treatment and recovery. Learning if your gut is healing can also be a reassuring step toward well-being. If you struggle communicating this to loved ones, talking to family about your gut needs is vital for support. Finally, consider hidden food intolerances as a possible cause of these symptoms.