The intricate relationship between humans and their resident microbes is rapidly reshaping our understanding of health and disease. For decades, microbiology focused largely on pathogenic organisms – those that cause illness. However, we now recognize a vast community of microorganisms, collectively known as the microbiome, residing within and on us, playing crucial roles in maintaining homeostasis. This microbial ecosystem isn’t merely present; it actively participates in fundamental physiological processes, from nutrient absorption to neurological function. Perhaps nowhere is this interplay more evident than in the respiratory system, where constant interaction between microbes, immune cells, and host tissues dictates both health and susceptibility to disease.
The respiratory tract isn’t a sterile environment. From the nasal passages down to the lungs, it’s colonized by diverse microbial communities – bacteria, viruses, fungi, even archaea – forming a dynamic ecosystem influenced by factors like age, genetics, geography, diet, and antibiotic use. This microbiome profoundly impacts the development and function of mucosal immunity, which serves as the first line of defense against inhaled pathogens. A balanced microbiome contributes to robust immune responses, preventing overreaction (leading to inflammation) or under-reaction (allowing infection). Disruption of this balance – termed dysbiosis – is increasingly linked to a spectrum of respiratory conditions, from allergies and asthma to chronic obstructive pulmonary disease (COPD) and even severe viral infections. Understanding the connection between liver health and immunity can further support overall immune function.
The Microbiome’s Influence on Mucosal Immunity
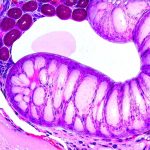
The development of mucosal immunity isn’t solely determined by genetics; it’s heavily sculpted by early microbial exposures. From birth onwards, colonization of the respiratory tract initiates a ‘training’ process for the immune system. This early exposure teaches the immune cells to distinguish between harmless commensals (the microbes that live peacefully with us) and dangerous pathogens. – The microbiome stimulates innate immunity: Microbial components like lipopolysaccharide (LPS) and peptidoglycan interact with pattern recognition receptors (PRRs) on immune cells, triggering responses such as cytokine production and phagocytosis – the engulfment and destruction of invaders. – It drives adaptive immunity: The microbiome influences the development of T cells and B cells, leading to antibody production and long-term immunological memory. This process is vital for effective defense against future infections.
Crucially, the microbiome doesn’t just activate the immune system; it also regulates it. Specific bacterial species can promote the generation of regulatory T cells (Tregs), which suppress excessive inflammation and maintain tolerance to harmless antigens. For example, certain bacteria produce short-chain fatty acids (SCFAs) through fiber fermentation – these SCFAs have potent anti-inflammatory properties and bolster Treg function. A healthy microbiome thus contributes to immune homeostasis, preventing both immunodeficiency and autoimmunity. This dynamic interplay is essential for a balanced respiratory immune response.
The composition of the gut microbiome also exerts surprising influence on respiratory immunity. The “gut-lung axis” refers to bidirectional communication between these two distant organs, mediated by various mechanisms including: – Immune cell migration – immune cells activated in the gut can travel to the lungs and vice versa. – Microbial metabolites – SCFAs produced in the gut can enter the bloodstream and affect lung immune function. – Systemic inflammation – dysbiosis in the gut can lead to systemic inflammation, impacting respiratory health. Therefore, interventions targeting the gut microbiome – such as dietary changes or probiotic supplementation – may have indirect but significant effects on respiratory immunity. Exploring nutrition myths about nausea can also help optimize gut health and overall wellbeing.
Microbial Metabolites and Immune Modulation
Microbial metabolites are small molecules produced by microbes during metabolism that act as signaling molecules influencing host physiology, including immune function. Beyond SCFAs, other microbial metabolites can significantly impact mucosal immunity. For instance: – Tryptophan metabolites: Gut bacteria metabolize tryptophan into compounds like indole derivatives which have anti-inflammatory properties and enhance barrier integrity. – Bile acid modifications: Gut microbes alter bile acids, impacting their signaling functions and influencing immune cell activity. – Polysaccharide A (PSA): Produced by Bacteroides fragilis, PSA has been shown to promote Treg development and reduce inflammation in various models.
The specific metabolites produced depend on the composition of the microbiome and dietary inputs. A diet rich in fiber promotes SCFA production, while a Western diet high in processed foods can lead to reduced microbial diversity and altered metabolite profiles. This highlights the critical role of nutrition in shaping both the microbiome and immune function. Understanding how different microbial metabolites modulate immunity is key to developing targeted therapies for respiratory diseases. The impact of irregular eating habits on digestive health should also be considered when optimizing dietary patterns.
The Role of Viruses in the Respiratory Microbiome
While bacteria often dominate discussions about the microbiome, viruses are integral components as well – particularly in the respiratory tract. The “virome” encompasses all viruses present, including bacterial viruses (bacteriophages), fungal viruses (mycoviruses) and eukaryotic viruses that can infect host cells. Bacteriophages, for instance, play a role in shaping bacterial community structure by selectively infecting and killing bacteria, thereby influencing the composition of the microbiome. This can have both positive and negative consequences depending on which bacteria are targeted.
The virome isn’t solely about pathogens; many viruses exhibit beneficial effects. Some viral infections can induce interferon production, enhancing antiviral immunity. Others may modulate immune cell function or promote barrier integrity. However, viral dysbiosis – an imbalance in the viral community – can contribute to respiratory disease exacerbations. For example, co-infections with multiple viruses or bacteria can overwhelm the immune system and lead to more severe outcomes. Research into the complex interplay between the bacterial and viral components of the respiratory microbiome is a rapidly evolving field.
Impact of Antibiotics on Microbial Balance & Immunity
Antibiotics, while life-saving in many cases, are notorious for their disruptive effects on the microbiome. Broad-spectrum antibiotics don’t discriminate between harmful bacteria and beneficial commensals, leading to collateral damage and reducing microbial diversity. This disruption can have profound consequences for mucosal immunity: – Reduced colonization resistance – a diminished ability of the microbiome to resist pathogen invasion. – Impaired immune development – disrupting the ‘training’ process for immune cells. – Increased susceptibility to infections – making individuals more vulnerable to respiratory pathogens.
The effects of antibiotics aren’t limited to the gut; they can also directly impact the respiratory microbiome, contributing to dysbiosis and weakening local defenses. Furthermore, antibiotic use has been linked to increased risk of asthma development in early life, possibly due to alterations in immune programming. Strategies to mitigate these adverse effects include: – Judicious antibiotic prescribing – using antibiotics only when necessary. – Probiotic supplementation – restoring beneficial bacteria after antibiotic treatment (though the efficacy varies depending on the strain and individual). – Fecal microbiota transplantation (FMT) – transferring a healthy microbiome from a donor to a recipient (primarily used for recurrent Clostridioides difficile infection, but research is exploring its potential in other conditions). The effects of antibiotics can significantly impact gut health.
Respiratory Infections & The Microbiome
The microbiome plays an active role during respiratory infections, influencing both the severity of illness and recovery. During viral infections like influenza or SARS-CoV-2, the microbiome can modulate immune responses to limit disease progression. A diverse and balanced microbiome may enhance antiviral immunity and reduce inflammation, leading to milder symptoms and faster clearance of the virus. Conversely, a dysbiotic microbiome can impair immune function and increase susceptibility to severe outcomes.
The microbiome also influences the secondary bacterial infections that often follow viral respiratory illnesses. Viral infection damages the airway epithelium, creating opportunities for bacterial colonization. A compromised microbiome may be less effective at preventing these secondary infections, leading to pneumonia or other complications. Understanding how the microbiome interacts with both viruses and bacteria is crucial for developing strategies to prevent and treat respiratory infections effectively. This includes exploring interventions that bolster microbial diversity and enhance immune function.
The specific changes in the microbiome during infection vary depending on the pathogen and individual factors. However, common observations include: – Decreased bacterial diversity. – Shifts in community composition – with an increase in opportunistic pathogens. – Altered metabolite profiles – reflecting changes in microbial metabolism. These alterations can create a vicious cycle of inflammation and immune dysfunction, exacerbating disease severity. Personalized approaches that take into account an individual’s microbiome profile may be necessary to optimize treatment strategies for respiratory infections. The connection between gut health and the body’s response to illness is crucial here. Dietary choices and even how to choose cookware can play a role in maintaining this balance. Finally, understanding nutrition myths about nausea can help support overall wellbeing during illness.