The gut microbiome – the vast ecosystem of trillions of bacteria, fungi, viruses, and other microorganisms residing in our digestive tract – is increasingly recognized as central to overall health. It’s not just about digestion anymore; this complex community profoundly influences immunity, mental wellbeing, nutrient absorption, hormone regulation, and even chronic disease risk. For a long time, understanding the specifics of an individual’s gut microbiome was challenging, relying mostly on symptoms and broad dietary recommendations. However, advancements in technology have made stool testing a powerful tool for peering into this hidden world, offering unprecedented insight into the composition and function of our gut flora. This allows for more personalized approaches to diet, lifestyle, and potentially targeted interventions aimed at optimizing digestive health and beyond.
Traditionally, assessing gut health involved focusing on symptoms like bloating, constipation, or diarrhea. While these are important indicators, they often represent downstream effects rather than root causes. Stool tests go further by directly analyzing the contents of our intestines, revealing what’s actually happening within the microbiome. They provide a snapshot of bacterial diversity, identify potential imbalances (dysbiosis), detect markers of inflammation, and assess digestive function. This detailed information empowers both individuals and healthcare practitioners to move beyond guesswork and develop more effective strategies for supporting gut health. It’s important to note that stool tests are not diagnostic tools in themselves; rather, they provide valuable data points that contribute to a broader assessment of overall wellbeing. Considering ways to reset your gut after dietary indulgences can be a good starting point.
Understanding the Scope of Stool Testing
Stool testing isn’t a single test but encompasses a variety of methodologies, each focusing on different aspects of gut health. Some tests utilize culture-based methods, attempting to grow and identify specific bacterial strains – this is often used for identifying pathogens or imbalances causing acute infections. However, many bacteria are difficult to culture, leading to an incomplete picture. More advanced techniques, like 16S rRNA gene sequencing and metagenomic sequencing, analyze the genetic material of the microbiome. This allows identification of a much wider range of microbial species, even those that don’t readily grow in a lab. The 16S technique focuses on a specific gene found in bacteria, while metagenomics analyzes all genetic material present, providing deeper insights into functional capabilities.
Beyond identifying who is living in your gut, some tests also assess what they are doing. This involves analyzing metabolites – the byproducts of microbial activity. For instance, short-chain fatty acids (SCFAs) like butyrate, propionate and acetate are produced when beneficial bacteria ferment fiber. SCFAs have numerous health benefits, including nourishing colon cells and reducing inflammation. Measuring SCFA levels can indicate the efficiency of your microbiome in breaking down fiber and producing these crucial compounds. Other metabolites assessed include bile acid markers, which reflect digestive function, and tryptophan metabolites, linked to brain health. You might also consider how to build a gut safe snack list as part of your dietary adjustments.
The increasing availability of at-home stool testing kits has democratized access to this information. While convenient, it’s vital to choose reputable companies that utilize validated methodologies and provide clear, actionable reports. Ideally, results should be reviewed with a qualified healthcare professional who can interpret the data in context and develop a personalized plan. Remember, a stool test is just one piece of the puzzle; integrating its findings with other health assessments – lifestyle factors, dietary habits, medical history – is crucial for comprehensive gut health management.
Decoding Key Markers in Stool Analysis
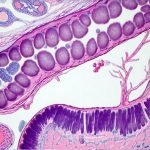
Stool tests often report on several key markers that provide valuable insights into gut function and microbial composition. – Alpha diversity measures the number of different species within a sample. Higher alpha diversity generally indicates a healthier, more resilient microbiome. – Beta diversity compares the overall similarity or dissimilarity between your microbiome and others, revealing how unique it is. – Specific bacterial abundance identifies which bacteria are present and in what quantities. Imbalances, known as dysbiosis, can involve an overgrowth of potentially harmful bacteria or a deficiency of beneficial ones.
Inflammation markers like calprotectin and lactoferrin indicate the level of inflammatory activity in the gut. Elevated levels may suggest conditions like Inflammatory Bowel Disease (IBD) or sensitivities to certain foods. It’s important to note that inflammation isn’t always negative; it’s a natural part of immune response, but chronic inflammation can be detrimental. Markers related to digestive function, such as pancreatic elastase and fecal fat content, assess how well your body is breaking down and absorbing nutrients. Low levels of pancreatic elastase could indicate insufficient pancreatic enzyme production, leading to malabsorption.
Finally, the presence of parasitic pathogens or opportunistic bacteria (those that can cause problems when their numbers become excessive) are also often assessed. Identifying these issues allows for targeted interventions like dietary changes, probiotic supplementation, or in some cases, prescribed medications. Understanding these markers requires expertise; a healthcare professional can help interpret results and determine the most appropriate course of action. It’s important to remember that individual ranges and interpretations can vary based on laboratory methodologies and population norms. If you have experienced years of reflux medication, exploring how to rebuild gut health is important.
The Role of Probiotics & Dietary Fiber
Stool test results frequently inform recommendations around probiotics – live microorganisms intended to benefit the host. However, probiotic supplementation isn’t a one-size-fits-all solution. A stool test can help identify specific bacterial deficiencies or imbalances, guiding the selection of probiotic strains that may be most beneficial for an individual. For instance, if a test reveals low levels of Bifidobacteria, a probiotic containing this strain might be recommended. It’s also crucial to consider that probiotics work best in conjunction with a supportive environment – namely, a diet rich in prebiotics.
Prebiotics are non-digestible fibers that serve as food for beneficial bacteria in the gut. Sources include onions, garlic, leeks, asparagus, bananas and oats. By providing fuel for these microbes, prebiotics encourage their growth and activity, enhancing the overall health of the microbiome. Dietary fiber is often categorized as soluble or insoluble; both types play a role in gut health but have different functions. Soluble fiber dissolves in water to form a gel-like substance, helping regulate blood sugar and cholesterol levels, while insoluble fiber adds bulk to stool and promotes regularity.
A comprehensive approach involves increasing dietary fiber intake gradually to avoid digestive discomfort. Stool tests can also assess the efficiency of fiber fermentation by measuring SCFA production. If SCFA levels are low despite adequate fiber consumption, it may indicate an issue with microbial diversity or function, prompting further investigation. The goal isn’t just about adding probiotics and prebiotics but rather cultivating a thriving gut ecosystem through a holistic approach encompassing diet, lifestyle, and stress management. You can also learn how to create a gut health routine for consistent support.
Integrating Stool Test Results into a Holistic Plan
Ultimately, the true value of stool testing lies in its ability to personalize gut health strategies. Results should be viewed as starting points for conversation with a healthcare professional, leading to tailored recommendations rather than rigid prescriptions. A plan might include dietary modifications – such as increasing fiber intake, reducing processed foods, or identifying and eliminating food sensitivities – along with targeted probiotic supplementation. Lifestyle factors like stress management, sleep hygiene, and regular exercise also play vital roles in gut health and should be addressed concurrently.
It’s important to remember that the microbiome is dynamic and constantly changing. Re-testing periodically can help track progress, assess the effectiveness of interventions, and adjust strategies as needed. This ongoing monitoring allows for a proactive approach to gut health management. The best approach isn’t simply fixing what appears broken but fostering a resilient and diverse gut ecosystem capable of adapting to challenges. Learning how to build a morning routine can set the tone for a healthy day.
Finally, while stool tests offer valuable insights, they should be part of a broader health assessment. Combining the data with information from blood tests, symptom tracking, and lifestyle evaluations provides a more comprehensive picture of overall wellbeing. By embracing this holistic approach, individuals can unlock the potential of their gut microbiome and optimize their health for years to come. If you plan on traveling, remember to build a travel kit!