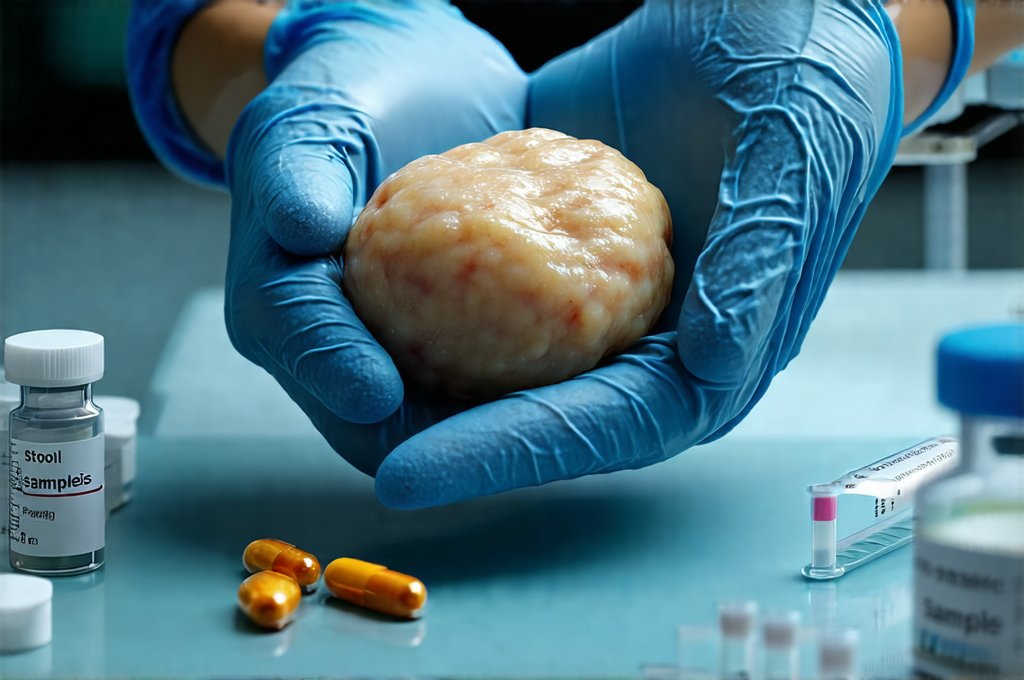
The pancreas, often overlooked yet undeniably vital, plays a dual role in our bodies – both as an endocrine organ regulating blood sugar and as a digestive organ producing enzymes that break down food. When things go awry with this complex organ, the consequences can be significant, impacting digestion, nutrient absorption, and overall health. Traditionally, diagnosing pancreatic issues has relied heavily on imaging techniques like CT scans and MRIs, endoscopic procedures, and blood tests measuring pancreatic enzymes. However, a relatively newer approach is gaining traction: analyzing stool samples. This seemingly simple method offers a non-invasive and increasingly accurate way to detect various pancreatic problems, providing valuable insights into its function and potential dysfunction.
For years, the focus has been on what’s happening inside the body – visualizing the pancreas directly or measuring enzyme levels in the blood. But now, we’re recognizing that the byproducts of pancreatic activity, specifically undigested fats and enzymes excreted in stool, can tell a compelling story about its health. Stool analysis doesn’t replace established diagnostic methods; instead, it complements them, often acting as an early warning system or helping to refine the diagnosis when other tests are inconclusive. This is particularly useful because some pancreatic conditions present subtle symptoms initially, making early detection crucial for better outcomes. If stress plays a role in your digestive issues, consider how a high-stress job might be impacting things.
The Role of Fecal Elastase-1 in Pancreatic Exocrine Insufficiency
Fecal elastase-1 (FE-1) is arguably the most important marker assessed in stool samples for diagnosing pancreatic exocrine insufficiency (PEI). This condition arises when the pancreas doesn’t produce enough digestive enzymes, leading to malabsorption of fats and nutrients. The beauty of FE-1 lies in its resilience; it’s a relatively stable enzyme that survives digestion remarkably well, making it an accurate indicator of pancreatic function. Unlike other pancreatic enzymes which can be affected by various factors, FE-1 levels directly reflect the amount of functioning pancreatic tissue.
Essentially, if the pancreas isn’t working efficiently, less elastase-1 will be present in the stool. Low FE-1 levels are highly suggestive of PEI, prompting further investigation. It’s important to note that a single low reading doesn’t definitively diagnose PEI; it often requires correlation with clinical symptoms and potentially other tests. However, FE-1 is considered a sensitive and specific marker for detecting even mild forms of PEI, which might otherwise go unnoticed until more serious complications arise. The test itself is straightforward: patients collect a small stool sample (typically following instructions to avoid contamination), which is then sent to a laboratory for analysis.
The interpretation of FE-1 results involves comparing the measured concentration to established reference ranges. Values below a certain threshold—generally around 50 μg/g feces—strongly suggest PEI and warrant further investigation into underlying causes like chronic pancreatitis, cystic fibrosis, or pancreatic cancer (though FE-1 is more reliable for detecting functional insufficiency than pinpointing the exact cause). Importantly, while high levels don’t necessarily indicate a healthy pancreas, they do suggest sufficient enzyme production. You might also consider if breathing exercises could help manage related discomforts.
Identifying Fat Malabsorption Through Stool Analysis
Beyond FE-1, stool samples can reveal evidence of fat malabsorption, a common consequence of PEI but also seen in other gastrointestinal disorders. When the pancreas doesn’t produce enough lipase (the enzyme that breaks down fats), or when there’s an issue with bile acid absorption, undigested fat ends up in the stool. This manifests as steatorrhea – fatty stools characterized by their pale color, unpleasant odor, and difficulty flushing.
Quantitative fecal fat testing measures the amount of fat excreted over a specified period (usually 72 hours) after consuming a standardized diet. This test requires meticulous collection and adherence to dietary guidelines for accurate results. However, newer, less burdensome methods are emerging. Qualitative assessments can be done visually – observing stool characteristics for excessive oiliness or greasiness. While subjective, this provides a preliminary indication of fat malabsorption that may prompt further, more precise testing.
- The presence of undigested fat globules in the stool is a visual clue to potential pancreatic dysfunction.
- Measuring fecal triglycerides and fatty acids offers another quantitative approach to assess fat absorption.
- Combining these assessments with FE-1 levels provides a comprehensive picture of pancreatic function and digestive capacity. This process can be affected by what you eat, so consider if a gut reset diet might offer some relief.
Detecting Pancreatic Enzyme Levels & Inflammation Markers
While FE-1 focuses on exocrine function, stool analysis can also offer insights into the presence of pancreatic enzymes themselves, albeit indirectly. Elevated levels of amylase or lipase in the stool aren’t typically used for initial diagnosis of acute pancreatitis (blood tests are preferred for that), but they can be helpful in chronic cases or when blood test results are ambiguous. However, these enzymes degrade quickly in the digestive tract so their detection is less reliable than FE-1.
More promisingly, research is exploring the use of stool samples to detect markers of inflammation related to pancreatic disease. Calprotectin, a protein released by neutrophils (a type of white blood cell) during inflammation, can be measured in stool and may indicate underlying inflammatory processes within the pancreas or surrounding tissues. While still an emerging area of research, elevated fecal calprotectin levels could potentially help differentiate between different causes of abdominal pain and identify individuals at risk for developing chronic pancreatitis.
Utilizing Stool Microbiome Analysis
The gut microbiome—the vast community of microorganisms living in our digestive tract—is increasingly recognized as a key player in overall health, including pancreatic function. Dysbiosis, an imbalance in the gut microbiome, has been linked to various gastrointestinal disorders and may even contribute to the development or exacerbation of pancreatitis. Stool microbiome analysis, using techniques like 16S rRNA gene sequencing, can identify the types and quantities of bacteria present in the gut.
- Specific bacterial imbalances have been observed in individuals with pancreatic disease, suggesting a potential link between microbiome composition and disease severity.
- Changes in the microbiome can influence inflammation, immune responses, and nutrient absorption – all factors relevant to pancreatic health.
- While still largely experimental, modulating the gut microbiome through dietary changes or probiotics might offer adjunctive therapies for managing pancreatic conditions. If you suspect a leaky gut is contributing to your symptoms, it’s worth exploring this further.
Limitations & Future Directions
Despite its growing utility, stool analysis isn’t a perfect diagnostic tool. The accuracy of FE-1 and other stool tests can be affected by several factors:
– Dietary intake: High fat diets can temporarily elevate fecal fat levels, potentially leading to false positives.
– Medications: Certain medications can interfere with enzyme activity or absorption.
– Collection methods: Improper collection techniques or contamination can compromise results.
Therefore, it’s crucial that stool samples are collected according to standardized protocols and interpreted in conjunction with clinical symptoms, medical history, and other diagnostic tests. Also, the technology is constantly evolving; newer assays and more sophisticated analytical techniques are being developed to improve the sensitivity and specificity of stool-based pancreatic diagnostics. Sometimes seemingly unrelated factors like diuretics can disrupt digestive processes, so awareness is key.
Looking ahead, researchers are investigating the potential of identifying specific microbial signatures associated with different types of pancreatic disease, allowing for earlier and more personalized diagnoses. Furthermore, combining stool analysis with other “omics” technologies – such as proteomics (studying proteins) and metabolomics (studying metabolites) – could provide a deeper understanding of the complex interplay between the pancreas, gut microbiome, and overall health. The future of pancreatic diagnostics is undoubtedly heading towards a more holistic and non-invasive approach, and stool analysis will likely play an increasingly important role in that evolution. Understanding gut health influences on overall wellbeing is crucial for proactive health management. Finally, consider if food rotation might help identify sensitivities impacting your digestion.