Chronic gut issues represent a significant challenge for both individuals experiencing them and healthcare professionals attempting to diagnose and manage them. Often, the journey to understanding these conditions isn’t straightforward; it’s rarely about a single definitive test result but rather an evolving picture constructed over time through repeated assessments. The complexity arises from the dynamic nature of the gut itself – its intricate microbiome, sensitive immune responses, and susceptibility to various internal and external factors. This means scan results, whether imaging technologies or specialized functional tests, don’t usually present as a clear ‘yes’ or ‘no’ diagnosis, but instead demonstrate shifts and changes that reflect the progression (or regression) of the underlying issue. Understanding how these scans evolve is crucial for personalized treatment strategies and realistic expectations throughout the healing process.
The difficulty in interpreting scan results stems partly from the fact that many chronic gut conditions share overlapping symptoms, making initial differentiation difficult. What might appear as irritable bowel syndrome (IBS) could potentially be linked to small intestinal bacterial overgrowth (SIBO), inflammatory bowel disease (IBD), or even food sensitivities – and these can coexist! Furthermore, the gut’s environment is constantly changing based on diet, stress levels, medication use, and myriad other influences. Therefore, a scan taken during a flare-up might show significantly different results than one taken during a period of relative calm. This necessitates ongoing monitoring to build a more complete understanding of the individual’s condition and tailor interventions accordingly. It’s vital to remember that scans are tools for understanding, not definitive labels. Considering factors like gut health influences can be incredibly helpful during diagnosis.
The Evolution of Imaging Results in Chronic Gut Issues
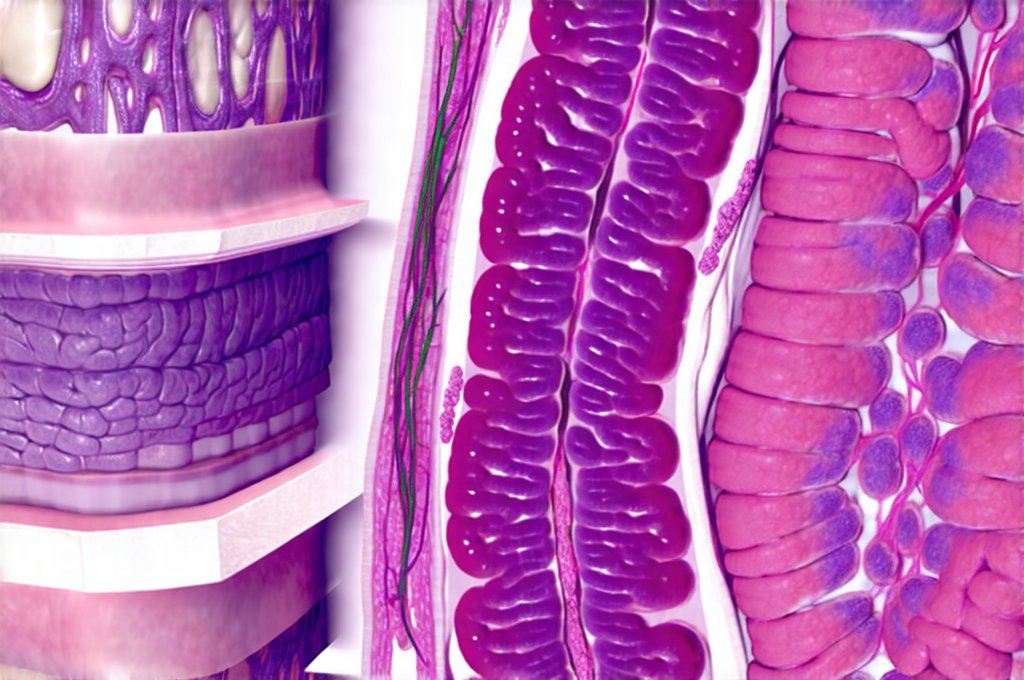
Imaging technologies like MRI, CT scans, and ultrasound play important roles in identifying structural abnormalities and inflammation within the digestive tract. However, their interpretation can be nuanced when dealing with chronic gut issues. In early stages, imaging might appear remarkably normal even while a patient is experiencing significant symptoms. This is common in conditions like functional dyspepsia or mild IBS where the issue isn’t necessarily related to physical damage but rather altered motility or visceral hypersensitivity. As the condition progresses – for example, transitioning from mild inflammation to more pronounced IBD – changes become visible on scans. These might include thickening of the intestinal wall, ulcerations, fistulas, or strictures.
The evolution isn’t always linear. Someone with Crohn’s disease, for instance, can experience periods of remission where imaging shows minimal evidence of active inflammation, followed by flare-ups where inflammation returns and scan results again demonstrate significant changes. It’s also important to note that different imaging modalities have varying sensitivities and specificities. An MRI might be better at detecting soft tissue inflammation, while a CT scan might excel at identifying structural damage. Therefore, the choice of imaging modality and how its results are interpreted should be guided by the suspected underlying condition and the patient’s individual symptoms. The trend over time – is inflammation increasing, decreasing, or remaining stable? – is often more informative than a single snapshot. Understanding colon transit time can also provide helpful context during this process.
Furthermore, ‘normal’ scan results don’t necessarily equate to complete health in chronic gut issues. A structurally normal bowel can still be functionally impaired. For example, someone with SIBO might have perfectly healthy-looking intestines on an MRI but exhibit abnormal breath test results indicating bacterial overgrowth. This highlights the need for a comprehensive assessment that combines imaging with functional testing and symptom evaluation.
Functional Gut Testing & Its Evolving Data
Functional gut tests aim to assess how the digestive system is working, rather than simply looking for structural abnormalities. These include tests like breath tests (for SIBO/IMO), stool analysis (to evaluate microbiome composition, markers of inflammation, and digestion/absorption), and intestinal permeability assessments (“leaky gut” testing). The results from these tests can also evolve significantly over time. Initial stool analysis might reveal a significant imbalance in the gut microbiome – for instance, low levels of beneficial bacteria and high levels of potentially pathogenic bacteria. As dietary changes are implemented, stress is managed, or targeted therapies (like probiotics) are used, subsequent stool analyses may demonstrate improvements in microbial diversity and abundance.
However, interpreting functional test results requires caution. The gut microbiome is incredibly complex and influenced by countless factors, so fluctuations are normal. A single stool analysis provides only a snapshot of the microbial community at that moment. Moreover, different labs use different methodologies for analyzing stool samples, leading to variations in results and interpretation. Breath tests for SIBO/IMO can also be prone to false positives or negatives depending on preparation protocols and individual physiology. The real value lies in tracking changes over time – are interventions leading to demonstrable improvements in gut function? Daily practices can significantly contribute to these positive shifts.
Understanding the Progression of Inflammation Markers
Inflammation is a common denominator in many chronic gut issues, even those that aren’t traditionally categorized as inflammatory bowel diseases. Assessing inflammation markers—in stool samples (calprotectin, lactoferrin) or blood tests (CRP, ESR)—provides valuable insight into disease activity and response to treatment. In early stages of IBD, for example, these markers may be mildly elevated but increase significantly during flare-ups. Conversely, successful treatment often leads to a reduction in inflammatory marker levels. It’s important to recognize that inflammation isn’t always bad; it’s part of the body’s natural healing process. However, chronic and uncontrolled inflammation can damage tissues and contribute to symptoms.
Tracking these markers over time allows healthcare professionals to assess the effectiveness of interventions and adjust treatment plans accordingly. For instance, if a patient is on anti-inflammatory medication but inflammatory markers remain elevated, it may indicate that the current dosage isn’t sufficient or that alternative therapies are needed. It’s also crucial to consider the context – inflammation can be influenced by factors outside the gut, such as infections, autoimmune conditions, or even psychological stress. A holistic approach is necessary for accurate interpretation.
The Role of Intestinal Permeability Testing Over Time
Intestinal permeability, often referred to as “leaky gut,” refers to increased gaps between the cells lining the intestinal wall. This allows undigested food particles, toxins, and bacteria to enter the bloodstream, potentially triggering immune responses and systemic inflammation. While controversial, testing for intestinal permeability (typically using a lactulose/mannitol breath test or zonulin levels in stool) can provide some insight into gut barrier function. In chronic gut issues, increased intestinal permeability often precedes and exacerbates symptoms.
As interventions aimed at healing the gut lining are implemented – such as dietary changes to reduce inflammation, supplementation with nutrients that support mucosal repair (like glutamine), or stress management techniques – subsequent tests may demonstrate improvements in intestinal permeability. However, like other functional tests, results can be variable. It’s crucial to remember that a “leaky gut” isn’t always the primary problem but often a consequence of underlying imbalances. Focusing solely on sealing the gut without addressing the root causes (such as chronic inflammation or dysbiosis) may not yield lasting results. Understanding gut permeability is crucial for effective treatment.
Interpreting Microbiome Analysis Trends
The gut microbiome is a complex ecosystem, and its composition can significantly impact overall health. Stool analysis can provide insights into microbial diversity, abundance of specific species, and presence of potential pathogens. In chronic gut issues, imbalances in the microbiome are common – for instance, reduced levels of beneficial bacteria like Bifidobacteria and Lactobacilli, and increased levels of opportunistic organisms. Tracking changes in microbiome composition over time is crucial for assessing the effectiveness of interventions such as probiotics, prebiotics, or dietary modifications.
However, it’s vital to avoid getting fixated on specific numbers or species. The “ideal” microbiome doesn’t exist – it varies from person to person based on genetics, diet, lifestyle, and other factors. Focus should be on overall microbial diversity and balance. An increase in diversity is generally considered a positive sign, indicating a more resilient and functional gut ecosystem. Furthermore, interpreting microbiome analysis requires considering the context of the individual’s symptoms and health history. A seemingly “unhealthy” microbiome may not necessarily be causing problems if the person isn’t experiencing any symptoms. Ultimately, the goal isn’t to achieve a perfect microbiome but rather to foster a thriving gut environment that supports optimal digestion, immunity, and overall well-being. Gut biofeedback can offer additional support in managing the gut’s response. Additionally, consider cooking hacks to improve tolerance. Understanding colon transit time can also be beneficial. Lastly, learn how to recognize a histamine reaction in the gut.