Gastroesophageal reflux disease (GERD), often simply called “acid reflux,” is an incredibly common condition affecting millions worldwide. While many associate it with a burning sensation in the chest – heartburn – the experience can be remarkably diverse, shifting throughout the day and presenting differently for each individual. This variability isn’t random; it’s deeply connected to our daily routines, body positions, dietary habits, and even hormonal fluctuations. Understanding how reflux symptoms change at different times of the day is crucial not just for managing discomfort but also for identifying potential triggers and tailoring effective lifestyle modifications or seeking appropriate medical guidance.
The frustrating aspect of reflux is its unpredictability. One person might struggle primarily at night, waking up with a sour taste in their mouth, while another experiences it most acutely after meals. Still others may find symptoms are worse during periods of stress or physical exertion. This article will explore the reasons behind these time-dependent variations, shedding light on why reflux behaves differently depending on when you experience it and what factors contribute to those changes. It’s important to remember that this information is for general knowledge purposes only and should not be substituted for professional medical advice. If you suspect underlying issues like rebuild trust it’s best to consult a doctor.
The Shifting Landscape of Reflux Throughout the Day
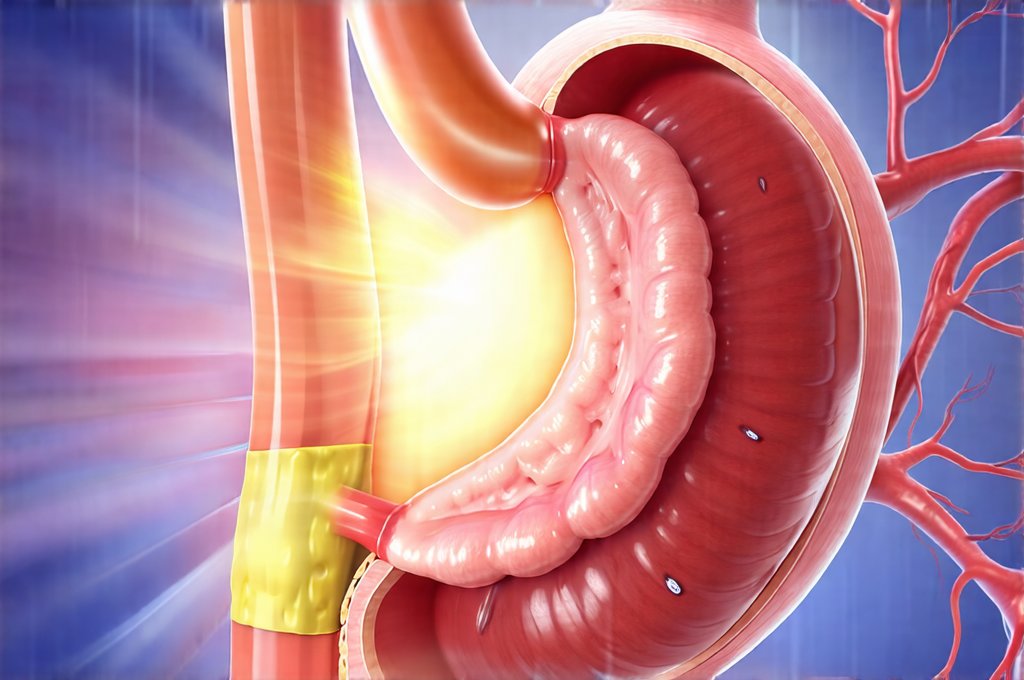
Reflux isn’t a constant state; it ebbs and flows with our daily activities. During the day, gravity generally works in your favor, keeping stomach acid where it belongs. When we’re upright, the lower esophageal sphincter (LES) – the muscle that acts as a barrier between the esophagus and the stomach – is naturally supported by body position. However, this advantage diminishes when we lie down or bend over. As such, daytime reflux often manifests differently than nighttime symptoms. Many individuals experience heartburn during or shortly after eating, particularly larger meals or foods known to trigger reflux (like spicy, fatty, or acidic items). This is because food volume can put pressure on the LES and increase stomach acid production. Other common daytime symptoms include regurgitation – the sensation of stomach contents coming back up into your throat – and a bitter or sour taste in the mouth. These are often more pronounced after meals and may be exacerbated by stress, which can affect digestive processes. Understanding how ibs symptoms flare up with stress is also important.
The type of activity also plays a significant role. Exercise, for instance, can sometimes worsen reflux, especially high-impact activities that increase abdominal pressure. Conversely, light walking can actually aid digestion and potentially reduce reflux symptoms in some individuals. Stressful situations frequently lead to increased stomach acid production and altered esophageal motility (the coordinated muscle contractions that move food down the esophagus), making daytime reflux more likely during periods of anxiety or tension. Furthermore, posture matters; slouching or bending over increases intra-abdominal pressure, pushing stomach contents upwards towards the LES. This explains why people often experience symptoms while working at a desk for extended periods or doing activities like gardening.
Finally, it’s important to note that daytime reflux isn’t always about acute flare-ups. Some individuals experience chronic, low-grade heartburn throughout the day, even without specific triggers. This can be indicative of more persistent underlying issues and warrants medical evaluation. Identifying these patterns is key to understanding your individual reflux experience and developing a targeted management plan. If you have fructose intolerance, learning how to reduce symptoms can also help manage overall digestive health.
Nighttime Reflux: A Different Beast Altogether
Nighttime reflux, also known as nocturnal reflux, presents a unique set of challenges compared to daytime symptoms. When we lie down, gravity no longer assists in keeping stomach acid contained. The LES is also more susceptible to relaxation during sleep. This combination significantly increases the risk of acid flowing back into the esophagus while you’re trying to rest. Consequently, nighttime reflux often manifests as silent reflux (Laryngopharyngeal Reflux or LPR) – symptoms that don’t involve typical heartburn but include things like chronic cough, hoarseness, sore throat, and even asthma-like symptoms. This is because the acid can irritate the larynx and upper respiratory tract without causing noticeable chest pain.
The horizontal position also allows stomach acid to remain in contact with the esophageal lining for a prolonged period during sleep, potentially leading to more significant irritation and damage. Unlike daytime reflux, which may be linked to specific meals, nighttime symptoms are often less predictable and can occur even on an empty stomach. This is because factors like delayed gastric emptying (how long food stays in the stomach) and fluctuations in hormone levels during sleep can influence acid production and LES function. Many people with nocturnal reflux experience difficulty sleeping due to discomfort or frequent awakenings caused by coughing, choking, or a burning sensation.
Managing nighttime reflux requires a multi-faceted approach that includes lifestyle modifications such as elevating the head of your bed (using blocks or a wedge pillow), avoiding late-night meals, and potentially adjusting medication timing in consultation with a doctor. It’s also crucial to identify any contributing factors like sleep apnea or obesity, which can worsen nighttime reflux symptoms. Recognizing gallbladder infection symptoms is important if you experience severe abdominal discomfort alongside reflux.
Understanding Triggers & Timing: Dietary Influences
Diet plays a monumental role in how reflux manifests throughout the day. Certain foods are well-known triggers, but timing matters just as much as what you eat. Large meals overwhelm the digestive system and put more pressure on the LES, increasing the likelihood of reflux regardless of the time of day. However, eating large meals close to bedtime is particularly problematic, as it gives the stomach less time to empty before lying down.
- Fatty foods: These slow down gastric emptying and promote LES relaxation.
- Spicy foods: Capsaicin, the compound that makes peppers spicy, can irritate the esophagus and increase acid production.
- Acidic foods & drinks: Citrus fruits, tomatoes, coffee, and carbonated beverages can directly irritate the esophageal lining.
- Chocolate: Contains compounds that relax the LES.
- Alcohol: Also relaxes the LES and increases stomach acid production.
Beyond these common triggers, individual sensitivities vary significantly. Keeping a food diary to track symptoms and identify personal trigger foods is an excellent starting point for dietary management. Furthermore, mindful eating – slowing down, chewing thoroughly, and avoiding distractions – can aid digestion and reduce reflux risk. Consider smaller, more frequent meals throughout the day instead of three large ones.
The Role of Body Position & Activity Level
As mentioned earlier, body position is a major determinant of reflux symptoms. Upright posture generally provides relief, while lying down exacerbates them. This explains why people often experience heartburn after bending over or slouching. However, even seemingly innocuous activities can contribute to reflux. Heavy lifting, strenuous exercise, and tight clothing all increase intra-abdominal pressure, potentially forcing stomach acid into the esophagus.
Consider these strategies:
1. Maintain good posture throughout the day.
2. Avoid lying down for at least three hours after eating.
3. Elevate the head of your bed by 6-8 inches.
4. Wear loose-fitting clothing.
5. Modify exercise routines to avoid high-impact activities immediately after meals.
Regular, moderate exercise is generally beneficial for overall health and can even help with digestion, but it’s important to choose activities that don’t worsen reflux symptoms. Light walking or yoga are often well-tolerated, while running or weightlifting might exacerbate the condition in some individuals.
Stress, Hormones & The Gut-Brain Connection
The link between stress and reflux is undeniable. When we experience stress, our bodies release hormones like cortisol, which can disrupt digestive processes and increase stomach acid production. Chronic stress can also lead to changes in esophageal motility, making it more difficult for food to move down the esophagus and increasing the risk of backflow.
Furthermore, hormonal fluctuations throughout the day can influence reflux symptoms. For example, progesterone levels rise during pregnancy, causing the LES to relax and increasing susceptibility to heartburn. Similarly, cortisol levels are naturally higher in the morning, which may contribute to increased acid production. The gut-brain connection is a two-way street; not only does stress impact digestion, but digestive issues can also affect mental health. Techniques for managing stress—such as meditation, deep breathing exercises, or yoga—can be valuable tools for reducing reflux symptoms and improving overall well-being. This interconnectedness highlights the importance of a holistic approach to reflux management that addresses both physical and emotional factors. Understanding why ibs and gas flare ups can also help manage stress related symptoms. Finally, consider if liver enlargement could be contributing to digestive discomfort.