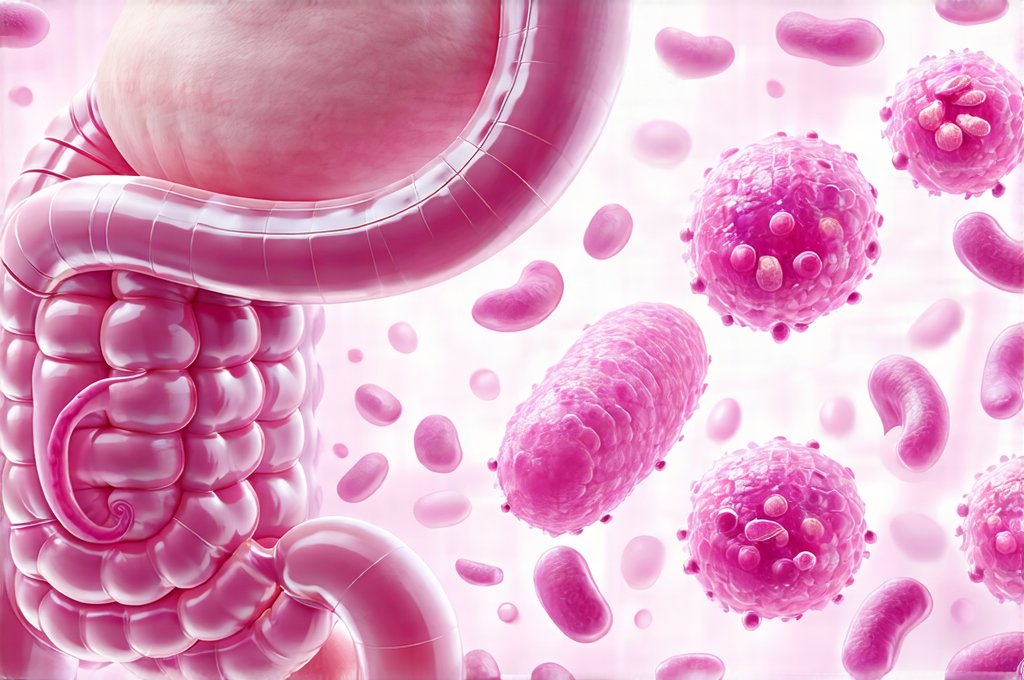
The digestive system is an incredibly complex ecosystem, constantly working to break down food, absorb nutrients, and eliminate waste. A crucial component of this system – and one often overlooked – is the gut microbiome: the trillions of bacteria, fungi, viruses, and other microorganisms that reside in our intestines. This microbial community isn’t just along for the ride; it actively participates in digestion, immune function, and even mental health. When this delicate balance is disrupted (by factors like antibiotics, diet, or stress), it can manifest as digestive issues, including changes to bowel movements. Increasingly, probiotics – live microorganisms intended to benefit the host – are being explored as a way to restore and maintain a healthy gut microbiome, potentially impacting everything from stool consistency to frequency.
Understanding how probiotics influence bowel function requires recognizing that “one size doesn’t fit all.” The gut microbiome is highly individualized, shaped by genetics, diet, lifestyle, and environment. Different probiotic strains have different mechanisms of action and therefore varying effects on the digestive system. What works for one person might not work for another. Furthermore, the relationship isn’t always direct; probiotics don’t necessarily cause a change in bowel movements but rather interact with existing gut flora to modulate the overall digestive process. This article will delve into the intricate ways probiotics can affect stool texture and frequency, exploring the underlying mechanisms and highlighting factors to consider when incorporating them into your routine.
The Impact of Probiotics on Bowel Frequency
Bowel frequency – how many times a day someone defecates – is highly variable and considered normal within a wide range (typically 3 times a day to 3 times a week). However, significant deviations from an individual’s usual pattern can be concerning. Probiotics can influence bowel frequency through several interconnected pathways. One key mechanism involves the production of short-chain fatty acids (SCFAs), like butyrate, acetate, and propionate, when probiotics ferment dietary fiber in the colon. SCFAs are not merely waste products; they’re vital for gut health, providing energy to colon cells, strengthening the intestinal barrier, and influencing motility. Increased SCFA production can stimulate colonic contractions, potentially leading to more frequent bowel movements – especially beneficial for individuals experiencing constipation.
Certain probiotic strains have been specifically linked to increased stool frequency in clinical studies. For example, Bifidobacterium lactis DN-173 010 has shown promise in easing occasional constipation and increasing the number of bowel movements per week. Similarly, some strains of Lactobacillus reuteri can accelerate colonic transit time, meaning food moves through the digestive system faster. Conversely, other probiotics might have a slowing effect. For instance, certain strains could help solidify stools by reducing inflammation or modulating gut motility, which could be helpful for individuals experiencing diarrhea. It’s crucial to remember this is strain-specific and not a universal effect.
The modulation of intestinal permeability – often referred to as “leaky gut” – also plays a role. A compromised intestinal barrier allows undigested food particles and toxins to enter the bloodstream, potentially triggering inflammation and affecting bowel function. Some probiotics can help strengthen the gut barrier by promoting the production of mucin (a protective layer lining the intestines) and tight junction proteins that hold cells together. A healthier barrier can lead to improved digestion and more regular bowel movements. Probiotic influence on frequency is also intertwined with hydration levels – adequate water intake remains paramount for healthy stool consistency, regardless of probiotic use. It’s important to consider how food temperature and pacing as well.
Understanding Constipation & Probiotics
Constipation, characterized by infrequent or difficult passage of stools, affects a significant portion of the population. It can be caused by various factors, including low fiber intake, dehydration, lack of physical activity, and certain medications. Probiotics don’t necessarily cure constipation but can act as an adjunct therapy to alleviate symptoms and improve regularity. The mechanism often involves increasing stool bulk and softening stools through SCFA production and increased water absorption in the colon.
- Studies have shown that specific strains like Bifidobacterium longum and Lactobacillus casei Shirota can be effective in reducing constipation severity and improving stool consistency.
- Probiotics might also help restore a healthy gut microbiome balance, which is often disrupted in individuals with chronic constipation. This restoration can improve the overall digestive process and promote regular bowel movements.
- It’s important to note that probiotics are generally more effective for functional constipation (related to lifestyle factors) than structural constipation (caused by anatomical issues). If indigestion plays a role, understanding acid exposure is important.
Probiotics & Diarrhea Management
Diarrhea, defined as frequent loose stools, can be equally disruptive. While often acute and self-limiting (e.g., from a viral infection), chronic diarrhea requires investigation. Probiotics can play a role in managing certain types of diarrhea, particularly antibiotic-associated diarrhea (AAD) – a common side effect of antibiotics that disrupts the gut microbiome. Saccharomyces boulardii, a probiotic yeast, is frequently recommended for AAD prevention and treatment due to its ability to counteract the negative effects of antibiotics on the gut flora and reduce inflammation.
- Probiotics can help restore the balance of gut bacteria after antibiotic use, reducing the overgrowth of harmful pathogens that contribute to diarrhea.
- Certain strains may also produce antimicrobial substances that inhibit the growth of diarrheal pathogens like Clostridium difficile (C. diff), a common cause of severe diarrhea.
- However, it is crucial to avoid using probiotics during acute infectious diarrhea without medical supervision, as they could potentially prolong symptoms in some cases. Stress and mental health can also contribute to digestive upset.
Probiotic Strain Specificity and Individual Responses
As mentioned earlier, the effect of probiotics on bowel movements is heavily strain-specific. Lactobacillus rhamnosus GG, for instance, has been shown to be beneficial for preventing diarrhea, but it might not have a significant impact on constipation. Similarly, Bifidobacterium infantis may improve symptoms in individuals with Irritable Bowel Syndrome (IBS), but its effects on bowel frequency can vary widely depending on the individual’s gut microbiome and IBS subtype. This highlights the importance of selecting probiotics based on specific needs and potentially consulting with a healthcare professional to identify appropriate strains.
Individual responses to probiotics are also highly variable. Factors like age, diet, genetics, pre-existing gut health, and concurrent medications can all influence how someone responds to probiotic supplementation. What works for one person might not work for another, even if they’re taking the same strain. It’s often necessary to experiment with different strains and dosages to find what works best for your body. Keeping a food diary and tracking bowel movements alongside probiotic use can help identify patterns and determine which probiotics are most effective. Understanding hormonal changes is also important when considering digestive issues.
Beyond Frequency: Probiotic Effects on Stool Texture
While frequency is an important aspect of bowel health, stool texture provides valuable insights into the overall digestive process. Ideal stool consistency falls somewhere between well-formed but soft – easily passed without straining. Probiotics can influence stool texture by altering water content, fiber fermentation, and gut motility. For example, probiotics that increase SCFA production can enhance water absorption in the colon, leading to firmer stools. Conversely, those that promote gut motility might result in softer stools.
A common issue is hard, dry stools associated with constipation. As discussed earlier, probiotics like Bifidobacterium lactis DN-173 010 can help alleviate this by increasing stool bulk and softening the stool through increased water content and SCFA production. However, it’s essential to address underlying causes of constipation, such as inadequate fiber intake or dehydration. On the other end of the spectrum, loose or watery stools are characteristic of diarrhea. Saccharomyces boulardii, along with specific strains of Lactobacillus, can help restore gut barrier function and reduce inflammation, leading to improved stool consistency.
The impact on stool texture is also related to the modulation of the gut microbiome’s composition. A diverse and balanced gut microbiome is associated with healthier stools. Probiotics can contribute to this diversity by introducing beneficial bacteria that compete with harmful pathogens and promote a more stable ecosystem. This stability, in turn, supports optimal digestion and absorption, leading to well-formed stools. The production of mucin, enhanced by some probiotics, further contributes to stool consistency by providing lubrication and aiding passage. Consider how food temperature impacts digestion as well.
It is crucial to remember that probiotics aren’t a quick fix for digestive issues. They work best as part of a holistic approach that includes a balanced diet rich in fiber, adequate hydration, regular physical activity, and stress management. If you are experiencing persistent or severe changes in bowel movements, it’s important to consult with a healthcare professional to rule out underlying medical conditions and receive personalized advice. GERD can also affect digestive health overall.