Gut pain – abdominal discomfort ranging from mild cramping to debilitating agony – is an incredibly common complaint. Many instances are easily attributable to identifiable causes like food poisoning, viral gastroenteritis, or dietary indiscretion. However, a significant number of individuals experience chronic or recurrent gut pain where standard tests and examinations yield no definitive diagnosis. This can be profoundly frustrating for patients, leading to anxiety, reduced quality of life, and a sense of being dismissed by healthcare providers. The challenge lies in the complexity of the digestive system itself, as well as the often subtle nature of underlying conditions that don’t readily appear on routine investigations. Effectively diagnosing these “functional” or poorly understood gut pain scenarios requires a careful and methodical approach, increasingly relying on advanced imaging techniques beyond traditional endoscopy and colonoscopy.
This article will explore how various imaging modalities are being utilized to help pinpoint the source of gut pain when conventional methods fall short. We’ll delve into the strengths and limitations of each technique, outlining what they can reveal about the structure and function of the digestive tract, and highlighting how this information aids in accurate diagnosis and appropriate management strategies. It’s important to emphasize that imaging isn’t always the answer; a thorough medical history, physical examination, and often trial-and-error approaches remain crucial components of care. However, when uncertainty persists, imaging can offer invaluable insights, bridging the gap between unexplained symptoms and informed clinical decision-making.
The Role of Structural Imaging: CT & MRI
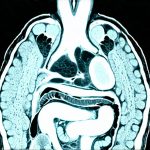
Computed Tomography (CT) scans and Magnetic Resonance Imaging (MRI) are foundational structural imaging techniques used extensively in evaluating gut pain. While both provide detailed anatomical images, they differ significantly in how those images are generated and what types of tissues they best visualize. CT scans use X-rays, making them relatively quick and inexpensive but exposing patients to ionizing radiation. They excel at visualizing bone structures, identifying obstructions within the bowel (like adhesions or tumors), and detecting acute inflammation associated with conditions like diverticulitis. MRI, on the other hand, utilizes magnetic fields and radio waves, avoiding radiation exposure altogether. It’s particularly strong in assessing soft tissues, making it ideal for evaluating inflammatory bowel disease (IBD), identifying subtle changes in the intestinal wall, and differentiating between various causes of abdominal pain.
The choice between CT and MRI often depends on the suspected underlying cause and patient-specific factors. For example, if a quick assessment is needed to rule out an emergency obstruction, a CT scan might be preferred. However, for a more comprehensive evaluation of chronic inflammation or to minimize radiation exposure in younger patients, an MRI would likely be favored. It’s also important to note that advanced CT techniques like CT enterography and MRI enterography specifically focus on the small bowel, which is often difficult to visualize with standard imaging methods. These specialized scans involve drinking a large volume of liquid containing contrast agents to distend the small intestine, allowing for better visualization of its walls and any potential abnormalities.
Modern imaging protocols also incorporate techniques like diffusion-weighted imaging (DWI) in MRI, which can help detect areas of inflammation or edema even before structural changes are visible on conventional scans. This is particularly useful in identifying early stages of IBD or distinguishing between active Crohn’s disease and quiescent disease. Ultimately, structural imaging provides a roadmap of the digestive tract, allowing clinicians to identify anatomical abnormalities that may be contributing to gut pain. Considering gut health alongside these findings can offer even more insight.
Functional Imaging: Unveiling Physiological Processes
While structural imaging tells us what is present in the abdomen, functional imaging reveals how things are working – assessing the physiological processes within the digestive system. This is crucial for diagnosing conditions where anatomical changes are minimal or absent, but function is impaired. One primary example of a functional imaging technique used to evaluate gut pain is breath testing. Although not typically considered “high-tech” like CT or MRI, it’s an incredibly valuable tool for identifying issues such as Small Intestinal Bacterial Overgrowth (SIBO) and lactose intolerance. Patients consume a specific sugar solution (like lactulose or glucose), and the amount of hydrogen gas exhaled is measured over several hours. Elevated hydrogen levels indicate bacterial fermentation in the small intestine, suggesting SIBO – a common cause of bloating, gas, and abdominal pain. If leaky gut is suspected, this can exacerbate symptoms.
Beyond breath testing, more advanced functional imaging techniques are emerging. Gastric emptying studies utilize radioactive tracers to measure how quickly food empties from the stomach into the small intestine. Delayed gastric emptying can contribute to nausea, vomiting, and upper abdominal discomfort, often seen in conditions like gastroparesis. Similarly, motility studies use sensors attached to the bowel or ingestible capsules equipped with pressure sensors to assess the speed and pattern of intestinal contractions. Abnormal motility can lead to constipation, diarrhea, or a combination of both, all contributing to gut pain. These functional assessments provide insights into how well the digestive system is processing food, identifying underlying issues that may not be visible on structural imaging alone.
Specialized Imaging for Specific Concerns
Small Bowel Evaluation: Capsule Endoscopy & Double Balloon Enteroscopy
The small bowel presents a unique diagnostic challenge due to its length and difficulty of access with traditional endoscopic methods. Capsule endoscopy involves swallowing a tiny wireless camera that travels through the entire digestive tract, transmitting images back to an external recorder. It’s particularly useful for detecting bleeding sources, identifying polyps or tumors, and assessing Crohn’s disease in the small intestine. However, it’s primarily diagnostic; there is no ability to take biopsies or perform therapeutic interventions with a capsule endoscope. Double balloon enteroscopy offers both diagnostic and therapeutic capabilities. It involves inserting a long, flexible endoscope through the mouth or rectum, utilizing balloons at each end to anchor the scope within the small bowel and navigate further down its length. This allows for visualization of the entire small intestine, as well as biopsy sampling and even treatment of bleeding sources.
Liver & Biliary Imaging: MRCP & Ultrasound
Gut pain can sometimes originate from structures adjacent to the digestive system, such as the liver, gallbladder, or pancreas. Magnetic Resonance Cholangiopancreatography (MRCP) is a specialized MRI technique that provides detailed images of the bile ducts and pancreatic duct without requiring invasive procedures like endoscopic retrograde cholangiopancreatography (ERCP). It’s used to identify gallstones, blockages, or inflammation within these ducts, which can cause referred pain in the abdomen. Ultrasound, while less precise than MRCP for visualizing deeper structures, is a readily available and inexpensive tool for assessing the gallbladder for stones or signs of acute cholecystitis (gallbladder inflammation). Combining structural and functional imaging, alongside clinical evaluation, allows for a comprehensive assessment of potential extra-intestinal causes of gut pain. It’s important to rule out other conditions like reflux which can sometimes mimic abdominal discomfort.
Peritoneal & Pelvic Imaging: Focused Attention on Hidden Issues
The peritoneum – the lining of the abdominal cavity – can be a source of chronic pain when inflamed or scarred. Identifying subtle peritoneal changes often requires high-resolution imaging and careful interpretation. Similarly, pelvic inflammatory disease (PID) or endometriosis in women can cause referred pain that mimics gut issues. MRI is particularly valuable in evaluating these conditions, providing detailed images of the pelvic organs and detecting adhesions or inflammation that may be contributing to pain. A holistic approach means considering all potential sources of abdominal discomfort, even those outside the digestive tract itself. Imaging plays a critical role in differentiating between these possibilities and guiding appropriate treatment strategies. Living with GI pain can be difficult, but imaging helps narrow down potential causes. If stress is a factor, consider high-stress jobs. Sometimes a gut reset diet can offer relief.
It’s crucial to remember that imaging is just one piece of the puzzle when diagnosing gut pain with no clear cause. A thorough medical history, physical examination, blood tests, stool analysis, and often trial-and-error approaches remain essential components of care. However, as imaging technology continues to advance, it offers increasingly sophisticated tools for unraveling the mysteries of the digestive system and providing relief for those suffering from unexplained gut pain. Gut parasites should also be considered as a potential cause.