Bloating and digestive discomfort are incredibly common experiences, affecting a large percentage of the population at some point in their lives. Often dismissed as minor inconveniences, these symptoms can significantly impact quality of life, ranging from mild annoyance to debilitating pain. While many factors contribute to bloating – diet, stress, food sensitivities, underlying medical conditions – one often overlooked yet crucial element is gut transit time. This refers to the amount of time it takes for food to move through your digestive system, and its influence on bloating isn’t simply about speed; it’s about balance. Too fast, and nutrients aren’t properly absorbed leading to fermentation; too slow, and waste products accumulate, again fostering bacterial overgrowth and gas production.
Understanding gut transit time is key to unlocking strategies for managing bloating because it directly impacts the microbial environment within your digestive tract. A healthy gut microbiome relies on a consistent flow of food, providing substrates for beneficial bacteria while preventing stagnation that favors undesirable microbes. When this process is disrupted – whether through rapid or sluggish movement – imbalances emerge, leading to increased gas production, inflammation, and ultimately, those uncomfortable bloating sensations. It’s not merely about what you eat, but how efficiently your body processes it.
The Science of Gut Transit Time
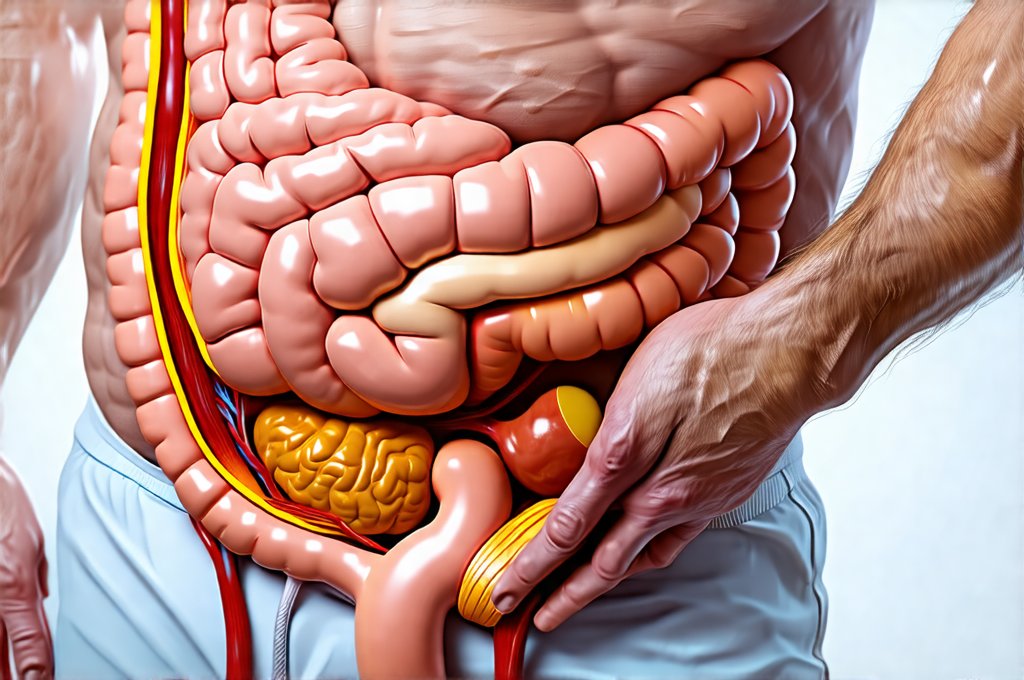
Gut transit time isn’t a single, fixed number; it varies significantly between individuals and is influenced by numerous factors. Generally, the entire process from ingestion to elimination should take anywhere from 24 to 72 hours. However, this encompasses several stages: oropharyngeal transit (mouth to esophagus), gastric emptying (stomach), small intestinal transit (digestion & absorption), and colonic transit (water absorption & waste formation). Each stage has its own typical timeframe, and disruptions in any one can cascade through the entire system. A ‘normal’ gut transit time is highly individualized, depending on factors like age, gender, activity level, diet composition, hydration status, stress levels, and even genetics.
The small intestine plays a pivotal role in this process; it’s where the majority of nutrient absorption happens. Food spends several hours here, allowing enzymes to break down complex carbohydrates and proteins. If food moves too quickly through the small intestine, nutrients aren’t fully absorbed, leading to fermentation by bacteria further down the line – resulting in gas and bloating. Conversely, if it lingers too long, bacterial overgrowth can occur, producing excessive amounts of gas as they ferment undigested material. The colon is responsible for water absorption; slow transit here leads to constipation and hardened stool, while rapid transit can result in diarrhea.
The microbiome itself is intimately linked to gut transit time. Certain microbial populations produce compounds that stimulate intestinal motility (movement), while others may have a slowing effect. This creates a complex feedback loop: the speed of food movement influences the microbiome, which then influences the speed of food movement. Maintaining a diverse and balanced microbiome is therefore crucial for regulating transit time and minimizing bloating. If you suspect issues with your gut, understanding gut microbiota can be helpful.
Factors Influencing Gut Transit Time
Numerous factors can disrupt the delicate balance of gut transit time, leading to either constipation or diarrhea – both contributing to bloating. Diet is arguably one of the most significant influencers. – A diet lacking in fiber slows down colonic transit time, increasing the risk of constipation and bacterial overgrowth. – High intake of processed foods, sugar, and unhealthy fats can also disrupt gut motility. – Conversely, excessive caffeine or alcohol consumption may speed up transit time, hindering nutrient absorption. Hydration is critical; dehydration slows down all stages of digestion.
Stress and anxiety are powerful modulators of digestive function. When stressed, the body diverts blood flow away from the digestive system to prioritize ‘fight-or-flight’ responses, slowing down motility. Chronic stress can lead to long-term disruptions in gut transit time. Physical activity plays a significant role; regular exercise stimulates intestinal contractions and promotes healthy movement. Finally, certain medications (opioids, antacids) and underlying medical conditions (irritable bowel syndrome, hypothyroidism) can also significantly impact gut transit time. It’s important to note that bloating and weight gain can sometimes be confused, so understanding the root cause is vital.
Assessing Your Gut Transit Time
While a formal diagnostic test requires medical evaluation, you can get a general idea of your gut transit time at home using a simple ‘food tracking’ method. This isn’t a substitute for professional advice, but it can provide valuable insights. 1. Eat a portion of indigestible fiber – corn or chia seeds work well because they are visibly identifiable in stool. 2. Record the exact time you consumed the fiber source. 3. Monitor your stools until you see the undigested fiber pass through. 4. The time elapsed between consumption and elimination represents your approximate gut transit time.
Keep in mind that this method provides a rough estimate, as it only measures colonic transit time (the final stage). Variations are normal. If consistently experiencing extremely rapid or slow transit times alongside significant bloating, seeking professional evaluation is vital to rule out underlying medical conditions. Focus on identifying patterns and making gradual dietary & lifestyle adjustments rather than fixating on specific numbers. It’s also useful to learn how reflux symptoms vary as these can sometimes mimic digestive issues.
Strategies for Optimizing Gut Transit Time
Optimizing gut transit time isn’t about forcing a specific speed; it’s about promoting healthy digestive function and restoring balance. A cornerstone of this is dietary modification. – Gradually increase fiber intake from whole foods (fruits, vegetables, whole grains) to support regular bowel movements. – Identify and eliminate food triggers that contribute to bloating. This might require an elimination diet under the guidance of a healthcare professional. – Stay adequately hydrated throughout the day.
Stress management techniques are also crucial – incorporating mindfulness, meditation, yoga, or deep breathing exercises can help regulate digestive function. Regular physical activity promotes intestinal motility. Probiotic-rich foods (yogurt, kefir, sauerkraut) and/or probiotic supplements can support a healthy microbiome. Prebiotics (found in garlic, onions, bananas) feed beneficial bacteria, further enhancing gut health. Finally, consider mindful eating practices – chewing food thoroughly and eating slowly aids digestion and reduces the burden on your digestive system. Remember that consistency is key; these strategies are most effective when implemented as part of a sustainable lifestyle. To maintain this improved transit time, it’s important to keep gut health simple. For those with limited time, you can still eat gut friendly! If you’re concerned about the difference between discomforts, understanding bloating and reflux discomfort can help narrow down the cause. Finally, remember to be aware of gut infections impact.