Gastroesophageal reflux disease (GERD) and sleep apnea are two distinct conditions that frequently co-exist, creating a complex interplay that can significantly worsen symptoms for those affected. Individually, both pose substantial challenges to overall health and well-being; GERD disrupts daily life with uncomfortable digestive issues, while sleep apnea fragments nighttime rest, leading to daytime fatigue and potential long-term health complications. However, when these conditions occur together, they often exacerbate each other in a cyclical fashion, making diagnosis and effective management more difficult. Understanding this relationship is crucial for individuals experiencing both ailments and for healthcare professionals seeking to provide comprehensive care.
The connection isn’t merely coincidental. Several physiological mechanisms link GERD and sleep apnea. Changes in pressure within the chest cavity during obstructive sleep events can contribute to acid reflux, while conversely, acid exposure from GERD can irritate the upper airway, potentially worsening breathing difficulties during sleep. This creates a feedback loop where one condition fuels the other, diminishing quality of life and increasing the risk of associated health problems like cardiovascular disease, asthma exacerbations, and even an increased risk of certain cancers over time. It’s important to note that this is not always a straightforward cause-and-effect relationship; rather it’s often a bidirectional association requiring careful evaluation.
The Interplay Between GERD and Sleep Apnea
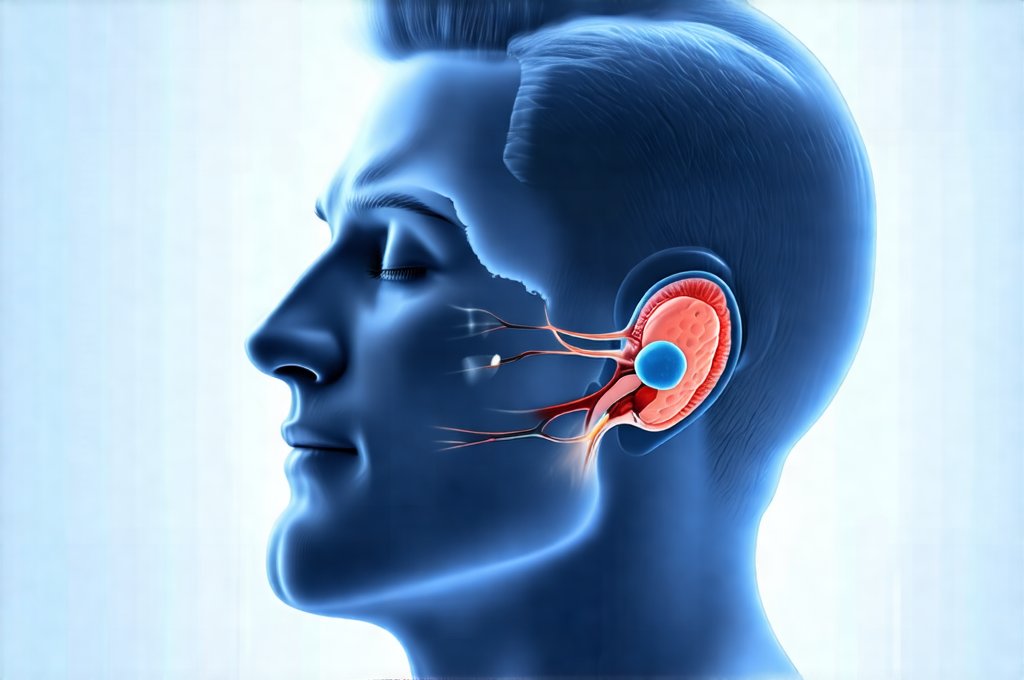
The fundamental issue lies in the disruption of normal physiological processes during sleep. Obstructive sleep apnea (OSA), the most common type, involves repeated episodes of upper airway collapse during sleep, leading to pauses in breathing. These events cause significant fluctuations in intrathoracic pressure – the pressure within the chest cavity. – Negative pressure created when attempting to breathe against a blocked airway can pull stomach acid up into the esophagus. – Conversely, positive pressure surges during resumption of breathing can also contribute to reflux. This mechanical stress on the lower esophageal sphincter (LES), the muscle that prevents stomach acid from flowing back up, weakens its function and makes it easier for acid to escape.
This relationship isn’t limited to OSA; central sleep apnea – though less common – can also play a role. The erratic breathing patterns associated with both forms of sleep apnea lead to arousal from sleep, disrupting normal sleep architecture. This fragmented sleep often leads to increased cortisol levels and altered digestive function, further exacerbating GERD symptoms. In essence, the act of sleeping—which should be restorative—becomes a trigger for both conditions. Furthermore, many individuals with GERD experience nighttime symptoms specifically because lying flat increases the likelihood of acid reflux; this is compounded by the pressure changes during sleep apnea events.
The presence of even mild GERD can significantly worsen sleep apnea symptoms. Acid reflux can irritate the vagus nerve which controls airway muscle tone and sensitivity, potentially leading to increased airway collapse and more frequent apneas. Chronic inflammation from acid exposure also contributes to swelling in the upper airway, further narrowing the passage and making obstruction more likely. It’s a vicious cycle: GERD worsens sleep apnea, and sleep apnea exacerbates GERD. This makes accurate diagnosis and tailored treatment essential for improving patient outcomes.
How Sleep Apnea Impacts GERD Symptoms
Sleep apnea doesn’t just contribute to GERD; it actively intensifies its symptoms. The repeated dips in oxygen levels (hypoxia) that characterize sleep apnea are linked to increased acid production in the stomach. While the exact mechanism is still under investigation, researchers believe hypoxia may stimulate gastric acid secretion and delay gastric emptying – meaning food stays in the stomach longer, increasing the chance of reflux. – This effect can be particularly noticeable for individuals who eat close to bedtime.
Beyond acid production, sleep apnea-induced fragmented sleep impacts digestive function overall. Poor sleep disrupts the natural circadian rhythms that regulate gut motility and enzyme secretion, leading to indigestion, bloating, and an increased perception of heartburn. The stress response triggered by frequent awakenings also contributes to heightened sensitivity to pain, making GERD symptoms feel more intense. This creates a scenario where individuals with both conditions may experience more severe and persistent digestive discomfort than those with either condition alone.
It’s important for patients experiencing chronic GERD to consider sleep apnea as a potential contributing factor, especially if their symptoms are worse at night or don’t respond adequately to traditional treatments like proton pump inhibitors (PPIs). A comprehensive evaluation, including a sleep study, can help determine if sleep apnea is present and guide appropriate management strategies. Understanding how enzyme deficiency affects digestion may also be helpful in these cases.
The Role of Lifestyle Factors
Lifestyle choices play a significant role in both GERD and sleep apnea, and addressing these factors can often improve symptom control. – Dietary modifications are crucial: avoiding trigger foods such as caffeine, alcohol, chocolate, fatty foods, and spicy dishes can reduce acid reflux episodes. – Maintaining a healthy weight is also essential; obesity is a major risk factor for both conditions. Even modest weight loss can significantly alleviate symptoms of sleep apnea and decrease the frequency of GERD flare-ups.
Regular exercise, when appropriate and under medical guidance, improves overall health and can promote better sleep quality. However, avoid exercising close to bedtime, as this can sometimes exacerbate reflux. – Elevating the head of the bed by six to eight inches can also help prevent nighttime acid reflux. This simple adjustment utilizes gravity to keep stomach acid from flowing back up into the esophagus during sleep. Smoking cessation is paramount, as smoking weakens the LES and irritates the esophageal lining. Considering how dairy affects mucus production can also inform dietary choices.
Treatment Approaches for Combined GERD & Sleep Apnea
Treating both conditions simultaneously is essential for achieving lasting relief. The cornerstone of sleep apnea treatment is often continuous positive airway pressure (CPAP) therapy – a device that delivers pressurized air through a mask to keep the airway open during sleep. CPAP has been shown to reduce acid reflux in some patients, likely by stabilizing intrathoracic pressure and improving oxygenation. – It’s crucial to find a properly fitted mask for optimal adherence.
For GERD, treatment typically involves lifestyle modifications, medications (such as PPIs or H2 receptor antagonists), and in some cases, surgical interventions. However, when combined with sleep apnea, the approach may need to be more nuanced. Simply suppressing acid production isn’t always enough; addressing the underlying sleep disorder is often critical for long-term success. – A collaborative approach between a gastroenterologist and a sleep specialist is ideal. How GERD affects your throat and voice should also be considered in treatment plans.
In some cases, optimizing CPAP settings can further reduce GERD symptoms. For example, increasing the IPAP (inspiratory positive airway pressure) setting may help counteract negative pressure during inhalation. Surgical options for GERD should be carefully considered in light of the patient’s sleep apnea status; certain procedures could potentially worsen breathing difficulties during sleep. Ultimately, a personalized treatment plan that addresses both conditions is vital for improving quality of life and preventing long-term health complications. How gallbladder removal affects pancreatic function can be relevant in some cases as well. It’s also important to remember that consistent follow-up with healthcare providers is key to monitoring progress and making necessary adjustments to the treatment regimen. How food sensitivities affect sleep quality might be a contributing factor for some patients. Furthermore, ensuring proper digestion with sleep hygiene is key to managing symptoms. Finally, understanding how fructose malabsorption affects energy levels can provide additional insight into overall well-being and potential contributing factors.