Gallbladder removal, known as cholecystectomy, is an increasingly common surgical procedure performed worldwide. Often necessitated by gallstones or gallbladder inflammation, it significantly alters the body’s digestive landscape. While many people experience minimal long-term effects after surgery, a substantial number report changes in their digestion – particularly concerning gas and bloating. Understanding why these changes occur requires a nuanced look at the gallbladder’s role in normal digestion, how its removal impacts bile flow, and what strategies can help mitigate uncomfortable symptoms. This isn’t merely about eliminating an organ; it’s about adapting to a new digestive reality.
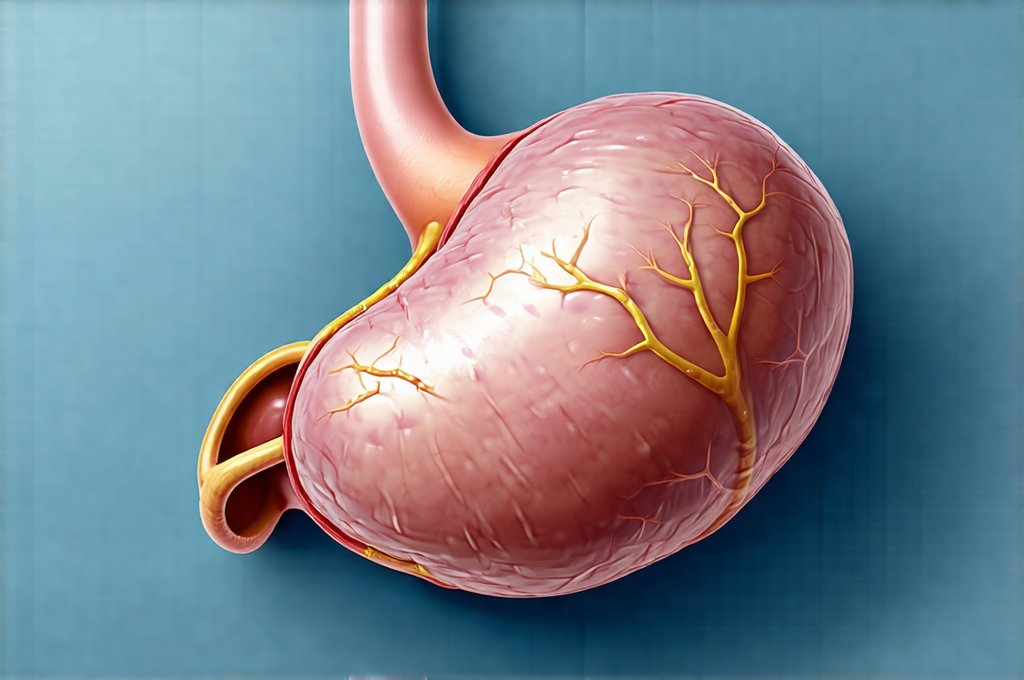
The gallbladder acts as a storage reservoir for bile, a fluid produced by the liver that plays a crucial part in fat digestion and absorption. When we eat, particularly foods containing fats, the gallbladder contracts and releases bile into the small intestine via the common bile duct. This emulsifies fats – breaking them down into smaller droplets – making it easier for enzymes to digest them. Removing the gallbladder doesn’t stop bile production; the liver continues to make it. However, without a storage system, bile drips continuously into the small intestine, rather than being released in concentrated bursts when needed. This constant flow can disrupt the digestive process and lead to various gastrointestinal symptoms, including increased gas production and altered bowel habits. Understanding how fast you eat can also impact these processes.
The Impact on Bile Flow and Fat Digestion
The most significant consequence of gallbladder removal is the change in bile delivery. Before surgery, bile was concentrated and released strategically; now it’s a constant, diluted stream. This impacts how efficiently fats are digested. Fats that aren’t properly emulsified can reach the large intestine where they become food for gut bacteria. The fermentation of undigested fat is a major contributor to gas production – specifically hydrogen, methane, and carbon dioxide. Individuals may notice increased flatulence, bloating, and even abdominal discomfort following meals containing higher amounts of dietary fat. The body must adapt to this altered process.
Furthermore, the continuous flow of bile can sometimes lead to bile acid diarrhea, a condition where excess bile acids irritate the colon. While not always directly causing gas, it can contribute to overall digestive distress and exacerbate feelings of bloating. The gut microbiome – the vast community of bacteria residing in our intestines – is also affected by this shift. Altered bile flow impacts the composition of these bacterial communities, potentially favoring species that produce more gas as a byproduct of their metabolic activities. It’s important to remember that each person’s gut microbiome is unique, meaning responses will vary considerably. Foods that cause gas can also exacerbate these issues.
The liver continues to produce bile post-cholecystectomy, but it may take time for its production to regulate itself optimally. Initially, the body needs to “learn” how to manage this continuous flow. Dietary adjustments play a key role in supporting this adaptation process. Reducing overall fat intake and choosing healthier fats can lessen the burden on the digestive system and minimize gas production. The goal isn’t necessarily to eliminate fat entirely, but to manage its quantity and quality.
Understanding Post-Cholecystectomy Syndrome
Post-cholecystectomy syndrome (PCS) refers to a collection of gastrointestinal symptoms that persist after gallbladder removal. It’s not uncommon – estimates suggest up to 30% of patients experience some degree of PCS. Gas, bloating, abdominal pain, diarrhea, and indigestion are all common manifestations. It’s crucial to differentiate between normal adaptation periods and persistent syndrome requiring medical attention. Symptoms typically peak within the first few weeks post-surgery and gradually improve over several months as the body adjusts. However, if symptoms persist or worsen beyond a reasonable timeframe, further investigation is warranted. How reflux symptoms can also influence the experience of PCS.
PCS isn’t necessarily caused by a single factor; it’s often multifactorial. Possible contributing elements include: – Bile acid malabsorption – leading to diarrhea and potential gas production – Sphincter of Oddi dysfunction – affecting bile flow – Underlying irritable bowel syndrome (IBS) – exacerbated by the surgical change – Dietary intolerances – becoming more apparent post-surgery. Diagnosing PCS can be challenging, as symptoms overlap with other conditions. Physicians often use a process of elimination to rule out alternative causes and may employ diagnostic tests like HIDA scans or fecal bile acid measurements.
Managing PCS typically involves dietary modifications (discussed below), medications to alleviate specific symptoms (like bile acid sequestrants for diarrhea), and lifestyle adjustments. It’s essential to work closely with a healthcare professional to develop a personalized management plan. Ignoring persistent symptoms can significantly impact quality of life, so seeking appropriate care is vital.
Dietary Strategies for Gas Reduction
Diet plays an enormous role in managing gas and digestive discomfort after gallbladder removal. While there’s no one-size-fits-all approach, several dietary strategies can help minimize symptoms: – Gradual Fat Intake: Avoid large amounts of fat in a single meal; instead, distribute fat intake throughout the day. – Healthy Fat Choices: Opt for unsaturated fats like olive oil, avocado, and nuts over saturated and trans fats found in processed foods. – Fiber Management: While fiber is generally beneficial, excessive fiber can sometimes increase gas production. Introduce fiber gradually and monitor tolerance. – Low FODMAP Diet: For some individuals, a low-FODMAP diet (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, And Polyols) can reduce gas by limiting specific carbohydrates that ferment in the gut. How to plan balanced meals is especially important post-cholecystectomy.
Beyond these general guidelines, identifying individual food intolerances is crucial. Common culprits include: – Cruciferous Vegetables: Broccoli, cauliflower, cabbage – known for their gas-producing properties. – Beans and Legumes: Contain oligosaccharides that are difficult to digest. – Carbonated Beverages: Introduce excess air into the digestive system. – Artificial Sweeteners: Can cause fermentation in the gut. Keeping a food diary can help pinpoint which foods trigger symptoms.
A phased approach is often most effective. Start with small dietary changes and gradually introduce new foods while monitoring your body’s response. Consider consulting with a registered dietitian to develop a personalized nutrition plan tailored to your specific needs and tolerances. Hydration also plays a key role – drinking adequate water helps keep things moving through the digestive system.
Lifestyle Adjustments and Gut Health Support
Beyond diet, several lifestyle adjustments can support digestive health after gallbladder removal. Regular physical activity promotes gut motility and reduces bloating. Stress management techniques like yoga or meditation can help regulate digestion as stress often exacerbates gastrointestinal symptoms. Chewing food thoroughly aids digestion by breaking down food into smaller particles. Eating slowly and mindfully allows your body to signal fullness, preventing overeating which can overwhelm the digestive system.
Supporting gut health is paramount. Probiotics – live bacteria that benefit the intestinal microbiome – may help restore balance and reduce gas production. Probiotic supplements or fermented foods like yogurt (if tolerated) are good sources. However, it’s important to choose a probiotic strain appropriate for your needs as different strains have different effects. Prebiotics – fibers that feed beneficial gut bacteria – can also be helpful.
Long-term digestive health requires a holistic approach. This includes addressing dietary factors, managing stress, incorporating regular exercise, and nurturing the gut microbiome. It’s about creating an environment where your digestive system can thrive despite the absence of the gallbladder. Remember to communicate openly with your healthcare provider about any persistent or worsening symptoms; they can provide guidance and ensure you receive appropriate care. Gallbladder removal affects other digestive organs, too. Also, overeating affects digestion overall. Lastly, remember that GERD and sore gums can be related to digestive issues.