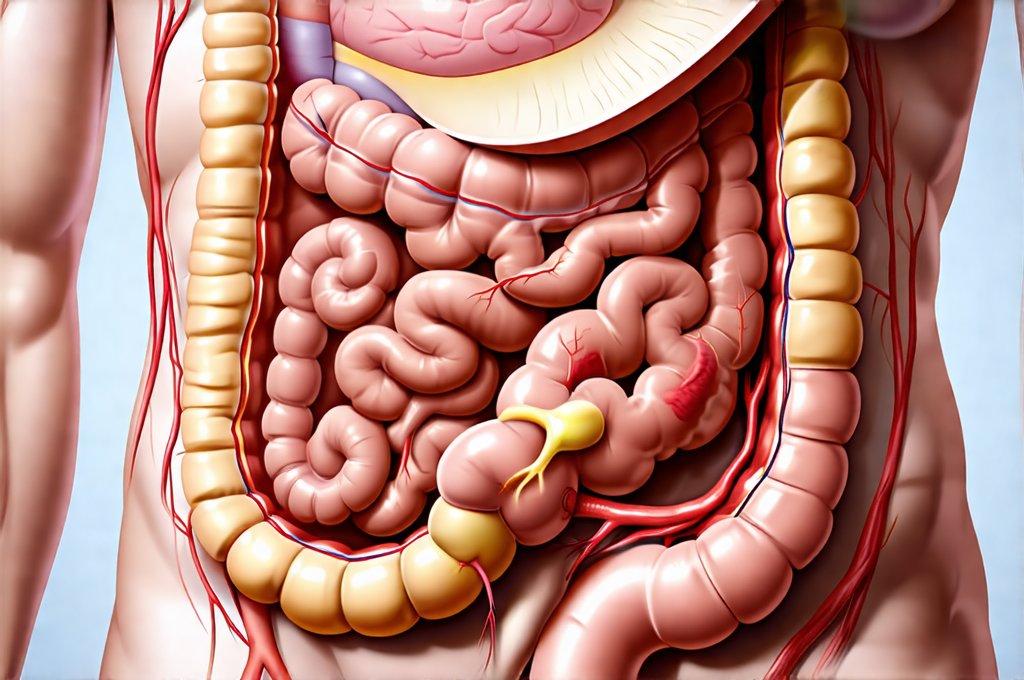
The gut – often referred to as our ‘second brain’ – is far more than just a digestive system. It’s a complex ecosystem teeming with trillions of microorganisms, collectively known as the gut microbiome, which profoundly impacts everything from immunity and mental health to nutrient absorption and chronic disease risk. Understanding the dynamic nature of this internal world—how it changes over time due to diet, lifestyle, medication, and even aging—is crucial for proactive healthcare. Historically, assessing gut health was limited to evaluating digestive symptoms. Today, however, a sophisticated toolkit is emerging that allows doctors to track these subtle but significant shifts in your gut’s composition and function with increasing precision, moving beyond simply treating problems to actively managing long-term gut wellness.
This ability to monitor the gut isn’t just about identifying illness; it’s about personalized medicine. Each individual’s microbiome is as unique as a fingerprint, influenced by genetics, environment, and personal habits. Tracking these changes allows healthcare professionals to tailor interventions – dietary adjustments, probiotic supplementation, or lifestyle modifications – to optimize your specific gut ecosystem and promote overall health. The exciting developments in this field are reshaping how we approach preventative care and chronic disease management, moving towards a more holistic understanding of the interconnectedness between our gut and our wellbeing.
Traditional & Modern Methods of Gut Assessment
For decades, doctors relied primarily on clinical evaluation and basic tests to assess gut function. This included detailed patient history focusing on symptoms like bloating, gas, constipation, or diarrhea, along with physical examinations to identify areas of tenderness or discomfort. Stool tests were often used, but initially focused on detecting pathogens (bacteria causing infection) rather than the broader microbiome composition. Fecal occult blood tests could indicate bleeding in the digestive tract, while stool cultures identified specific infectious agents. However, these methods provided a limited snapshot and didn’t reveal much about the vast community of microorganisms residing within us.
Modern advancements have revolutionized gut assessment. We now have techniques that allow for far more detailed analysis of the microbiome. These include: – 16S rRNA gene sequencing: This method identifies different bacterial species present in a stool sample by analyzing a specific gene sequence found in bacteria. It provides a comprehensive overview of microbial diversity. – Whole-genome shotgun metagenomic sequencing: A more advanced technique that sequences all the DNA in a stool sample, offering even greater detail about microbial composition and functional potential (what the microbes are capable of doing). – Metabolomics: This analyzes the metabolic byproducts produced by gut bacteria, providing insights into their activity and how they’re influencing your health. – Breath tests: Used to detect imbalances like Small Intestinal Bacterial Overgrowth (SIBO), where excessive bacteria in the small intestine ferment carbohydrates, producing gases that can be detected in breath samples.
These modern techniques are not just more accurate; they also provide a dynamic picture of gut health. Repeated testing allows doctors to track changes over time and assess the impact of interventions like dietary changes or probiotic supplementation. The ability to identify imbalances early on is critical for preventing chronic disease and promoting long-term wellbeing, moving beyond reactive treatment towards proactive management of gut health. Understanding gut tolerance is vital in this process.
Tracking Inflammatory Markers in Gut Health
Inflammation plays a central role in many gut disorders and systemic diseases. Chronic inflammation within the gut can be caused by factors like an imbalanced microbiome, leaky gut syndrome (increased intestinal permeability), or food sensitivities. Doctors utilize several methods to track inflammatory markers as indicators of gut health over time. C-reactive protein (CRP) is a common blood test that measures general inflammation in the body and can be elevated in cases of gut inflammation. However, it’s not specific to the gut.
More targeted assessments include: – Fecal calprotectin: A protein released by white blood cells during inflammation in the intestines. It’s measured in stool samples and is highly sensitive for detecting intestinal inflammation, particularly in conditions like inflammatory bowel disease (IBD). Repeated fecal calprotectin testing can help monitor disease activity and response to treatment. – Stool biomarkers: Some advanced stool tests measure specific markers of inflammation, such as lactoferrin and secretory IgA (sIgA), providing further insights into gut immune function. – Blood tests for antibodies: In cases of suspected food sensitivities or autoimmune conditions affecting the gut, blood tests can identify antibodies against specific foods or intestinal tissues, indicating an inflammatory response.
Tracking these markers over time allows doctors to assess the effectiveness of interventions aimed at reducing inflammation, such as dietary changes, probiotic supplementation, or anti-inflammatory medications. A consistent decrease in inflammatory markers suggests improvement in gut health and a reduction in disease risk. It’s important to note that inflammation is a complex process and these markers are just one piece of the puzzle—they should be interpreted alongside clinical symptoms and other diagnostic tests. How GERD can impact your health also plays a role in inflammation levels.
The Role of Diet & Lifestyle Tracking
While sophisticated testing methods provide valuable information, they’re often used in conjunction with careful tracking of diet and lifestyle factors. What you eat profoundly impacts your gut microbiome, and understanding these connections is crucial for personalized interventions. Doctors may recommend keeping a detailed food diary to identify potential trigger foods or dietary imbalances that might be contributing to gut symptoms. This isn’t just about eliminating certain foods; it’s about identifying patterns and making informed choices to support a healthy microbiome.
Lifestyle factors also play a significant role. Stress, sleep deprivation, and lack of physical activity can all negatively impact gut health. Doctors may ask patients to track: – Stress levels: Using questionnaires or journaling techniques. – Sleep quality: Monitoring sleep duration and disruptions. – Physical activity: Tracking exercise frequency and intensity. – Medication use: Including antibiotics, which can significantly disrupt the microbiome.
By correlating these lifestyle factors with gut symptoms and test results, doctors can develop a more comprehensive understanding of an individual’s gut health and tailor interventions accordingly. For example, if a patient reports high stress levels and consistently experiences bloating after consuming certain foods, a recommendation might include stress management techniques alongside dietary adjustments to reduce inflammation. The emphasis is on creating sustainable lifestyle changes that support long-term gut wellness. Meal spacing strategies can also greatly influence digestion and overall health.
Emerging Technologies & Future Directions
The field of gut health tracking continues to evolve rapidly with exciting new technologies emerging. Gut microbiome transplantation (GMT) is gaining traction as a treatment for recurrent Clostridioides difficile infection and shows promise for other conditions, requiring careful monitoring of donor and recipient microbiomes over time. Advances in artificial intelligence (AI) are also being applied to analyze complex microbiome data and predict individual responses to interventions with greater accuracy.
Furthermore: – Continuous glucose monitors (CGMs) can now provide insights into how different foods impact blood sugar levels and potentially gut health, as imbalances in the microbiome can affect glucose metabolism. – Smart toilets equipped with sensors are being developed to automatically collect stool samples for analysis, providing a non-invasive way to track changes in the microbiome over time. – Personalized probiotics: Based on an individual’s specific microbiome profile, tailored probiotic formulations may be designed to address imbalances and promote optimal gut health.
These advancements promise to further refine our understanding of the gut ecosystem and enable even more personalized and effective interventions. The future of gut health tracking is focused on moving beyond reactive treatment towards proactive management and prevention—empowering individuals to take control of their wellbeing through a deeper understanding of this vital internal world. Can your gut get used to sensitive foods over time? And what role does voice change play in gut health? Finally, consider incorporating some helpful cooking hacks into your daily routine.