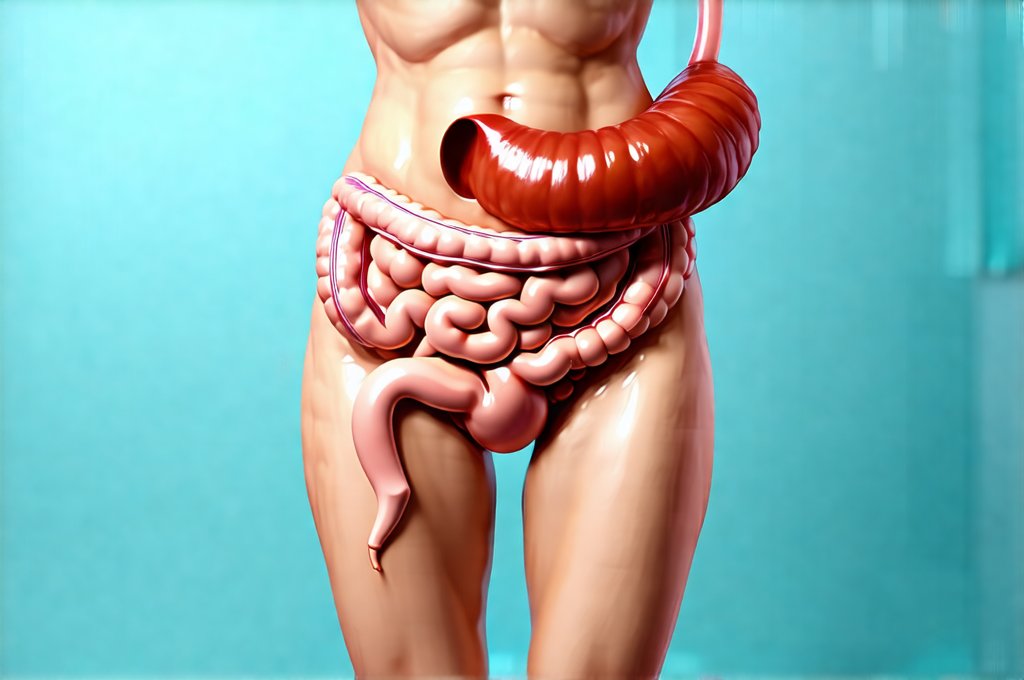
Following an illness – even something as seemingly mild as a cold or flu – it’s incredibly common to experience lingering digestive discomfort. Many people find themselves battling bloating, gas, constipation, or a general feeling of ‘fullness’ long after the initial symptoms have subsided. This isn’t necessarily alarming; it’s often a natural consequence of how our bodies respond to illness and recovery. The immune system, when activated, shifts resources away from typical bodily functions like digestion, prioritizing defense mechanisms. Consequently, digestive processes can slow down considerably, creating an environment where things don’t move as smoothly through the gut.
This temporary slowdown isn’t simply a matter of reduced enzyme production or decreased peristalsis (the wave-like muscle contractions that move food along). It’s also linked to changes in the gut microbiome, our complex community of intestinal bacteria. Illness, and often the treatments used to combat it (like antibiotics), can disrupt this delicate balance, impacting digestion and leading to increased gas production. The interplay between a weakened digestive system and an altered microbiome is frequently at the root of post-illness bloating, making understanding these mechanisms crucial for effective relief and restoration of gut health.
Understanding Digestive Sluggishness Post-Illness
Digestive sluggishness after illness isn’t a single phenomenon; it’s a cascade of interconnected events. When your body is fighting off infection, blood flow is redirected to support the immune system, meaning less goes to the digestive tract. This reduction in blood supply impacts several key processes: – Reduced enzyme production necessary for breaking down food. – Slower peristalsis, leading to prolonged transit time (how long it takes food to move through your system). – Decreased stomach acid production, hindering initial stages of digestion.
The result is that food isn’t properly broken down and absorbed, leaving more undigested material in the colon. This creates a breeding ground for gas-producing bacteria. Furthermore, inflammation – a natural part of the immune response – can linger even after the illness itself has passed, further contributing to digestive upset. The gut lining might become temporarily more permeable (often referred to as ‘leaky gut’ although this term is controversial), potentially triggering additional discomfort and bloating. This isn’t necessarily permanent damage but rather a temporary state that requires supportive care. It can be helpful to understand how to recover from these flare ups.
The type of illness also plays a role. Viral infections, for example, can directly impact the cells lining the digestive tract, leading to transient malabsorption. Bacterial infections may necessitate antibiotic use, which as mentioned earlier, significantly disrupts the gut microbiome. Even seemingly unrelated illnesses like upper respiratory infections can indirectly affect digestion due to stress and altered lifestyle factors (like changes in diet or activity levels). The body’s overall energy expenditure during illness further contributes to digestive slowdown; it simply doesn’t have the resources to maintain optimal function while simultaneously battling infection. If you find your digestive system is often stressed, consider how to reduce stress after periods of intense strain.
How the Gut Microbiome is Affected
The gut microbiome is arguably the most significant factor in post-illness bloating. A healthy gut microbiome boasts a diverse range of bacterial species, each playing a vital role in digestion, immunity, and overall health. Antibiotics, frequently prescribed to treat bacterial infections, are notoriously indiscriminate – they kill both harmful and beneficial bacteria. This disruption leads to dysbiosis: an imbalance in the gut microbial community.
Dysbiosis can manifest in several ways that contribute to bloating. – An overgrowth of gas-producing bacteria. – A reduction in bacteria responsible for breaking down complex carbohydrates, leading to fermentation and increased gas. – Impaired production of short-chain fatty acids (SCFAs), essential compounds for gut health and motility. The diminished SCFA production slows down colon contractions and promotes inflammation. Restoring microbial balance is therefore paramount for alleviating post-illness bloating. Taking steps to support enzyme production can also aid digestion.
Beyond antibiotics, even viral infections can indirectly impact the microbiome by altering the gut environment. Changes in diet during illness – often leaning towards easily digestible foods that lack fiber – further exacerbate dysbiosis. Stress, a common companion to illness, also negatively affects the microbiome composition. The goal isn’t necessarily to ‘rebuild’ the microbiome from scratch, but rather to create an environment where beneficial bacteria can thrive and outcompete harmful ones. This is achieved through dietary modifications (see below) and potentially probiotic supplementation after consulting with a healthcare professional. It’s also important to remember how to support gut healing generally.
Dietary Strategies for Relief
Diet plays a central role in managing post-illness bloating. The goal isn’t necessarily to eliminate entire food groups, but rather to prioritize easily digestible foods that support gut healing and minimize gas production. Here are some key strategies: 1. Focus on Low-FODMAP Foods: FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, And Polyols) are types of carbohydrates that can be poorly absorbed in the small intestine, leading to fermentation and bloating. Temporarily reducing high-FODMAP foods like onions, garlic, apples, wheat, and dairy can provide significant relief. 2. Increase Soluble Fiber Intake: Soluble fiber absorbs water in the gut, creating a softer stool and promoting regular bowel movements. Good sources include oats, bananas, berries, and psyllium husk. Introduce soluble fiber gradually to avoid exacerbating bloating initially.
- Hydrate Adequately: Water is essential for healthy digestion and prevents constipation, which can worsen bloating. Aim for at least 8 glasses of water per day. Beyond hydration, consider incorporating ginger or peppermint tea into your routine; these have traditionally been used to soothe digestive discomfort. It’s also important to avoid processed foods, sugary drinks, and excessive caffeine, as these can further irritate the gut. The key is mindful eating – paying attention to how different foods affect your body and adjusting accordingly. You may find it helpful to reduce bloating by carefully monitoring what you eat.
Gentle Movement & Stress Management
While it might seem counterintuitive when you’re feeling unwell, gentle movement can actually aid digestion and reduce bloating. Light exercise, like walking, yoga, or stretching, stimulates peristalsis and helps move gas through the digestive tract. Avoid strenuous activity, as this can put additional stress on your system. Regular physical activity also supports overall gut health and reduces inflammation.
However, don’t underestimate the power of stress management. Stress has a profound impact on digestion, often slowing it down or causing muscle tension in the gut. Techniques like deep breathing exercises, meditation, mindfulness, or spending time in nature can help reduce stress levels and improve digestive function. Chronic stress significantly impacts the microbiome as well, making stress reduction an essential component of post-illness recovery. Remember how minor daily stress can affect digestion.
It’s important to remember that post-illness bloating is often a temporary condition. With patience, mindful self-care, and appropriate dietary adjustments, most people experience significant improvement within a few weeks or months. If symptoms persist or worsen despite these efforts, it’s essential to consult with a healthcare professional to rule out any underlying conditions. Remember: your gut health is interconnected with your overall wellbeing. Taking proactive steps to support it will not only alleviate bloating but also enhance your long-term health and resilience. Finally, if you are reintroducing foods after illness, how to reintroduce fiber can be a useful resource.