Gastroesophageal reflux disease (GERD) is an incredibly common condition, affecting millions worldwide. Most people experience occasional heartburn, that burning sensation in the chest after eating, but GERD signifies a more chronic and severe form of acid reflux. It’s not simply about discomfort; prolonged, untreated GERD can lead to significant health complications, and one of the most concerning is an increased risk of esophageal cancer. Understanding this connection – how frequent acid exposure damages the esophagus over time, potentially leading to cancerous changes – is crucial for proactive healthcare and early detection. This article will delve into the relationship between GERD and esophageal cancer, exploring the mechanisms involved, identifying risk factors, and outlining strategies for management and prevention.
The concern isn’t that all individuals with GERD will develop esophageal cancer; in fact, the vast majority won’t. However, the chronic inflammation and cellular changes caused by persistent acid exposure can create a fertile environment for malignant transformation in some cases. It’s vital to differentiate between occasional heartburn and diagnosed GERD, as well as to recognize the symptoms that warrant medical attention. This isn’t about inducing panic; it’s about empowering individuals with knowledge so they can advocate for their health and make informed decisions regarding lifestyle modifications, treatment options, and regular screenings when appropriate. Early detection remains the single most important factor in improving outcomes for esophageal cancer, making awareness of this link incredibly valuable. Understanding the role of support groups https://vitagastro.com/understanding-the-role-of-support-groups-for-cancer-survivors/ can provide valuable emotional support during this journey.
Understanding the Link Between GERD and Esophageal Cancer
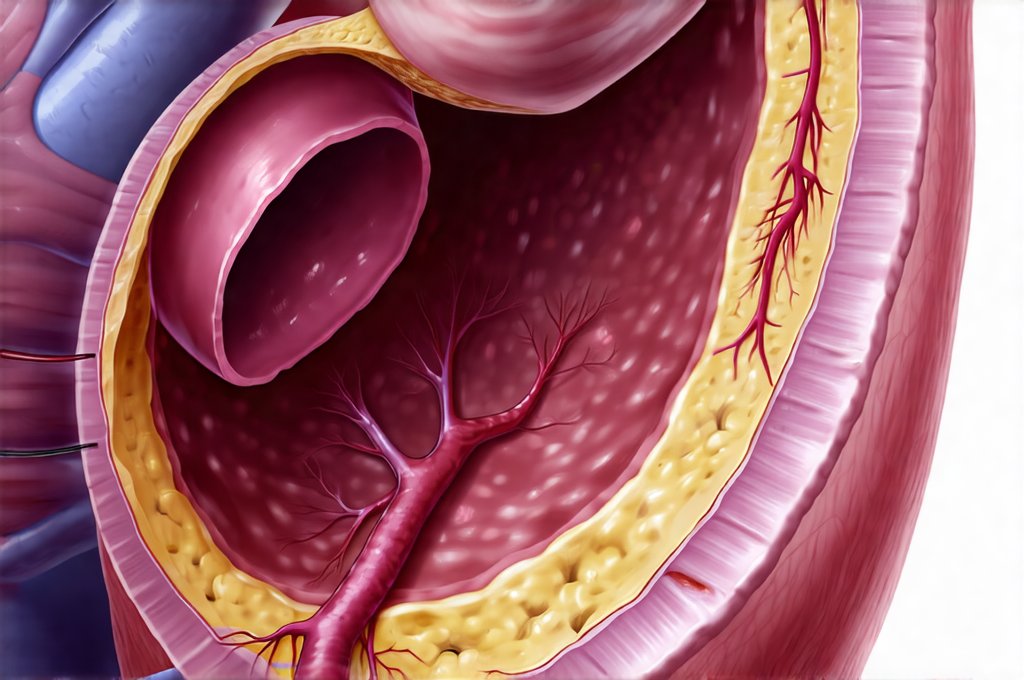
The connection between GERD and esophageal cancer isn’t straightforward; it’s not a direct cause-and-effect relationship. Instead, chronic GERD can lead to changes in the esophagus that increase the risk of developing certain types of this cancer. Specifically, the most common type linked to GERD is adenocarcinoma, which arises from glandular cells in the lower portion of the esophagus. This link centers around a precancerous condition called Barrett’s esophagus. When stomach acid frequently flows back into the esophagus over years, the normal squamous cell lining can be replaced by intestinal-type cells – this is Barrett’s esophagus. While Barrett’s itself isn’t cancer, it significantly elevates the risk of developing adenocarcinoma.
The process unfolds gradually. Frequent acid reflux causes chronic inflammation and damage to the esophageal lining. This ongoing irritation prompts the body to attempt repair, often leading to metaplasia (the change from squamous cells to intestinal-type cells). Barrett’s esophagus is diagnosed through endoscopy with biopsies; it’s estimated that approximately 1% – 5% of people with GERD will develop Barrett’s. However, only a small percentage of those with Barrett’s ultimately progress to esophageal adenocarcinoma. It’s important to remember this progression isn’t inevitable, and regular surveillance is key for early detection of any concerning changes. The impact of cancer on digestive function https://vitagastro.com/understanding-the-impact-of-cancer-on-digestive-function/ can significantly affect quality of life, highlighting the importance of preventative measures.
This risk isn’t limited solely to the presence of Barrett’s esophagus. Even in the absence of diagnosed Barrett’s, long-standing GERD can contribute to cellular damage that increases cancer susceptibility. The constant cycle of acid exposure, inflammation, and attempted repair creates a microenvironment prone to genetic mutations over time. Therefore, effectively managing GERD symptoms is critical not just for relieving discomfort but also for potentially reducing the long-term risk of esophageal cancer development. Nutritionists in cancer https://vitagastro.com/understanding-the-role-of-nutritionists-in-cancer-care/ can provide personalized dietary guidance to support overall health and potentially reduce cancer risk.
Barrett’s Esophagus: A Precursor Condition
Barrett’s esophagus represents a crucial turning point in the GERD – esophageal cancer pathway. It’s often asymptomatic, meaning individuals can have it without realizing anything is wrong. This underscores the importance of screening for those at higher risk (chronic GERD sufferers, especially men and those with long-standing symptoms). Diagnosis occurs via endoscopy, where a thin, flexible tube with a camera is inserted into the esophagus to visualize the lining. Biopsies are then taken to determine if metaplasia has occurred and, if so, to grade the extent of changes within the Barrett’s tissue.
There are different grades of dysplasia (abnormal cell growth) within Barrett’s esophagus: – No Dysplasia – indicates intestinal metaplasia without significant cellular abnormalities. Requires ongoing surveillance but lower risk. – Low-Grade Dysplasia – mild cellular changes; increased monitoring and potential treatment options. – High-Grade Dysplasia – more significant cellular changes, a very strong precursor to cancer, often requiring intervention like ablation or surgery.
Regular endoscopic surveillance is essential for individuals diagnosed with Barrett’s esophagus. The frequency of these screenings depends on the grade of dysplasia present. For example, those with high-grade dysplasia will require much closer monitoring and potentially immediate treatment to prevent progression to adenocarcinoma. Surveillance allows doctors to detect early signs of cancerous changes and intervene promptly, significantly improving prognosis. Cancer caregivers https://vitagastro.com/understanding-the-role-of-caregivers-in-cancer-care/ play a vital role in supporting patients through this process, offering emotional and practical assistance.
Risk Factors for GERD-Related Esophageal Cancer
While GERD is a key factor, several other risk factors contribute to the development of esophageal cancer in individuals with this condition. Age plays a role; the incidence of both GERD and esophageal adenocarcinoma increases with age, typically diagnosed over 55. Gender is also significant – men are disproportionately affected compared to women, though rates are increasing among women. Lifestyle factors like obesity and smoking exacerbate the risk, as they can worsen GERD symptoms and contribute to cellular damage.
Beyond these individual factors, certain demographic groups exhibit higher incidence rates of esophageal adenocarcinoma. White males, in particular, have shown a significant increase in diagnosis over the past few decades. This may be related to lifestyle changes and dietary habits within this population. Family history is also important; having a first-degree relative with esophageal cancer increases your personal risk.
Finally, chronic Helicobacter pylori infection – though more strongly linked to stomach cancer – can influence GERD symptoms and potentially impact the development of Barrett’s esophagus. It’s crucial to discuss all relevant health factors with your physician when evaluating your individual risk profile for esophageal cancer. Understanding these combined influences allows for a more targeted approach to prevention and early detection. The financial impact of treatment https://vitagastro.com/understanding-the-financial-impact-of-cancer-treatment/ can be a significant concern for many patients, making it important to plan accordingly.
Management and Prevention Strategies
Managing GERD effectively is paramount in mitigating the risk of progressing towards esophageal cancer. This often involves a multi-faceted approach, starting with lifestyle modifications: – Dietary Changes: Avoiding trigger foods (spicy, fatty, acidic), eating smaller meals, avoiding late-night eating, and elevating the head of your bed during sleep. – Weight Management: Losing weight if overweight or obese can reduce pressure on the stomach and esophagus. – Smoking Cessation: Smoking weakens the lower esophageal sphincter, worsening reflux.
Medications play a crucial role in controlling acid production. Proton pump inhibitors (PPIs) are commonly prescribed to significantly reduce stomach acid levels, while H2 receptor antagonists offer another option, though generally less potent. It’s important to use these medications under medical supervision as long-term PPI use can have potential side effects. Finally, for some individuals with severe GERD unresponsive to medication, surgical intervention like fundoplication (strengthening the lower esophageal sphincter) might be considered.
Regular endoscopic surveillance is vital for those diagnosed with Barrett’s esophagus. This allows for early detection of dysplasia and prompt treatment if necessary. Ablation techniques like radiofrequency ablation (RFA) can effectively remove abnormal tissue, preventing progression to cancer. In summary, proactive management of GERD symptoms, coupled with regular screening when appropriate, represents the most effective strategy for reducing the risk of esophageal cancer development. Remember that this is about empowering yourself through knowledge and working collaboratively with your healthcare provider to create a personalized plan tailored to your individual needs and risk factors. Understanding the role of diet in recovery https://vitagastro.com/exploring-the-role-of-diet-in-cancer-recovery/ can also significantly impact a patient’s well-being and long-term health outcomes. Finally, it’s important to understand the impact of diet https://vitagastro.com/impact-of-diet-on-the-risk-of-developing-gi-cancers/ on the risk of developing GI cancers in general.