Gastroesophageal reflux disease (GERD) is a surprisingly common condition affecting millions worldwide, often presenting as frequent heartburn or acid indigestion. While many associate GERD solely with excessive stomach acid, the reality is far more nuanced. Increasingly, healthcare professionals are recognizing a strong interplay between GERD and food intolerance symptoms, suggesting that what appears to be simple digestive discomfort could actually stem from a complex interaction between reflux and individual sensitivities to certain foods. This connection isn’t always straightforward – it’s not simply about acidic foods triggering reflux; instead, the body’s inflammatory response to intolerant foods can exacerbate GERD symptoms or even be misidentified as GERD itself. The link between food reactions may also contribute to other issues.
Understanding this link is crucial for effective management because traditional GERD treatments (like proton pump inhibitors) don’t always address the root cause when food intolerance plays a significant role. Many individuals continue to suffer despite medication, often unknowingly exacerbating their issues by continuing to consume trigger foods. The overlap in symptoms – bloating, gas, abdominal pain, nausea – makes accurate diagnosis challenging, demanding a holistic approach that considers both reflux and potential food sensitivities. This article will explore the intricate relationship between GERD and food intolerance, providing insights into identifying possible triggers and navigating a path toward improved digestive health. If you struggle with this, it may be helpful to understand the connection between mood and your symptoms as well.
Understanding the GERD-Food Intolerance Connection
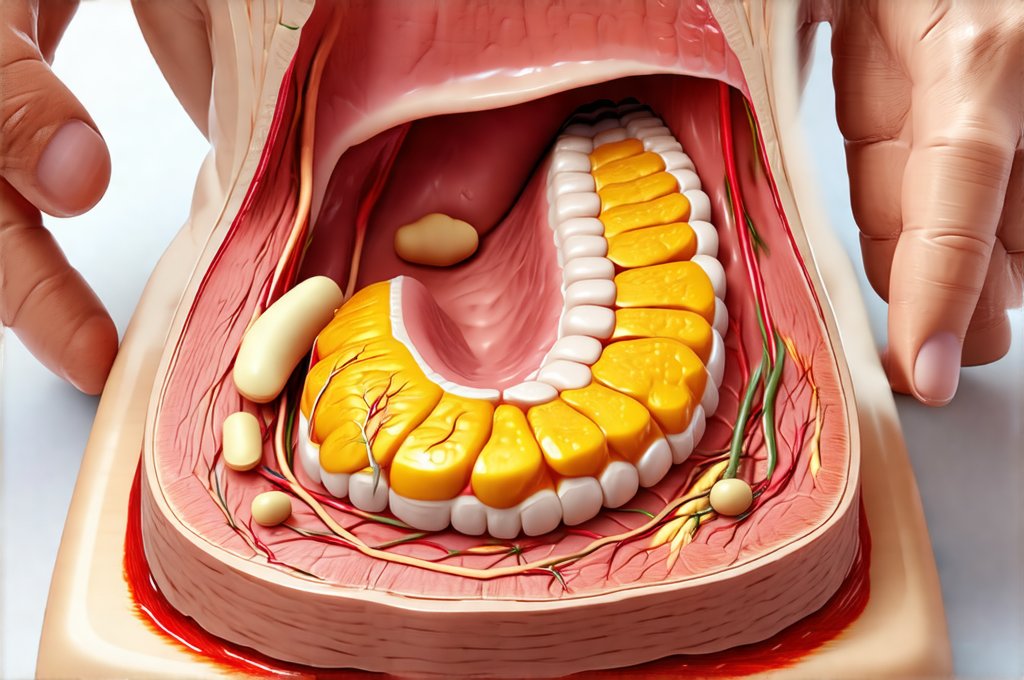
GERD arises when stomach acid frequently flows back up into the esophagus, irritating its lining. Normally, the lower esophageal sphincter (LES) acts as a valve, preventing this reflux. However, factors like a weakened LES, hiatal hernia, or increased abdominal pressure can compromise its function. While diet is undeniably a factor – certain foods can relax the LES or increase acid production – it’s not always the whole story. Food intolerance, unlike food allergy, doesn’t involve an immune response (IgE antibodies); instead, it represents difficulty digesting specific components of food, leading to gastrointestinal distress. This digestive struggle can create a cascade of events that worsen GERD symptoms.
The relationship isn’t unidirectional. Reflux itself can contribute to inflammation in the esophagus and even higher up into the throat, potentially increasing sensitivity to certain foods. Someone who previously tolerated dairy without issue might find it problematic once GERD is present. Furthermore, chronic inflammation from food intolerance can weaken the LES over time, creating a vicious cycle of reflux and increased sensitivities. This explains why some individuals experience persistent GERD symptoms even with medication – they’re addressing the acid but not the underlying trigger contributing to inflammation and esophageal damage. Understanding esophagitis can also help you understand the process.
A key aspect of this connection lies in gut health. A disrupted microbiome (an imbalance of bacteria in the digestive tract) is frequently observed in both GERD sufferers and those with food intolerances. This disruption can impair digestion, increase intestinal permeability (“leaky gut”), and fuel systemic inflammation, all contributing to a worsening of symptoms for both conditions. It’s becoming increasingly clear that addressing gut health is paramount for long-term management.
Common Food Intolerance Culprits in GERD
Identifying food intolerances isn’t always easy, as reactions can be delayed or subtle. However, several foods are frequently implicated in exacerbating GERD symptoms, either directly through their impact on the LES or indirectly by triggering inflammation. Dairy is a common offender for many, due to lactose intolerance (difficulty digesting milk sugar) and/or sensitivity to dairy proteins. Gluten, found in wheat, barley, and rye, can also cause digestive distress and inflammation, particularly in individuals with non-celiac gluten sensitivity. Fatty foods are another frequent culprit – they delay stomach emptying, increasing the risk of reflux, and can also weaken the LES.
Beyond these common triggers, other foods to consider include: – Chocolate (contains compounds that relax the LES) – Caffeine (can increase acid production and relax the LES) – Spicy foods (irritate the esophageal lining) – Citrus fruits and juices (high acidity) – Tomatoes and tomato-based products (high acidity) – Carbonated beverages (increase abdominal pressure) – Alcohol (relaxes the LES). It’s important to remember that individual sensitivities vary greatly. What triggers one person might not affect another, emphasizing the need for personalized dietary exploration. You may even react differently over time to foods.
It’s crucial to differentiate between food intolerance and allergy. A true food allergy involves a rapid immune response and can be life-threatening; intolerances are generally less severe but still significantly impact quality of life. If you suspect a food allergy, seek immediate medical attention. For suspected intolerances, a systematic approach to elimination and reintroduction (described below) is often the most effective way to identify triggers.
Identifying Food Intolerances: A Step-by-Step Approach
Pinpointing food intolerances requires detective work. Simply eliminating all potential triggers isn’t sustainable or helpful – it deprives you of valuable information about what specifically affects you. The gold standard is often an elimination diet, guided by a healthcare professional if possible. Here’s how it typically works: 1. Elimination Phase: Remove suspected trigger foods from your diet for a defined period (typically 2-3 weeks). This requires diligent label reading and avoiding hidden sources of the culprit food. Keep a detailed symptom journal to track any changes in your GERD symptoms, bloating, gas, or other digestive issues. 2. Reintroduction Phase: Gradually reintroduce one suspected food at a time, observing for any return of symptoms. Introduce only one food every 3-4 days to accurately assess its impact. Again, meticulous symptom tracking is essential. 3. Confirmation & Adjustment: If a food consistently triggers symptoms upon reintroduction, it’s likely an intolerance. Continue avoiding that food and move on to testing another potential trigger.
It’s important to note that this process requires patience and consistency. Symptoms can be delayed, making accurate identification challenging. Consider working with a registered dietitian or nutritionist who specializes in gut health; they can provide personalized guidance and ensure you’re maintaining a nutritionally adequate diet during elimination and reintroduction phases. They can also help interpret your symptom journal and develop a long-term dietary plan that minimizes triggers without unnecessary restrictions. Breaking the cycle of avoidance is essential for improving quality of life.
The Role of Gut Health Testing
While an elimination diet is the cornerstone of identifying food intolerances, gut health testing can provide valuable additional information. Several types of tests are available, including stool analysis (to assess microbiome composition) and breath tests (to detect malabsorption of certain sugars like lactose). These tests aren’t perfect – they offer a snapshot in time and don’t always correlate directly with symptoms – but they can help identify underlying imbalances that contribute to both GERD and food intolerance.
For example, a stool analysis might reveal a deficiency in beneficial bacteria or an overgrowth of harmful bacteria, suggesting the need for probiotic supplementation or dietary changes to support microbiome health. A breath test could confirm lactose malabsorption, guiding dietary modifications. It’s essential to discuss gut health testing with your doctor to determine if it’s appropriate for your situation and to interpret the results accurately. Remember that tests should be used as part of a broader assessment, not as a replacement for careful symptom tracking and dietary experimentation.
Beyond Diet: Lifestyle Factors & GERD Management
While food intolerance plays a significant role, managing GERD effectively requires addressing lifestyle factors too. Maintaining a healthy weight is crucial, as excess abdominal pressure increases the risk of reflux. Avoid eating large meals, especially before bedtime. Elevate the head of your bed by 6-8 inches to help prevent nighttime reflux. Quit smoking and limit alcohol consumption, both of which can weaken the LES. Stress management techniques, such as yoga or meditation, can also be beneficial, as stress can exacerbate GERD symptoms.
Finally, consider the timing of meals and medications. Avoid lying down for at least 3 hours after eating. If you’re taking medication for GERD, follow your doctor’s instructions carefully. Remember that medication should ideally complement dietary and lifestyle changes, not replace them entirely. A holistic approach – addressing both reflux and potential food sensitivities – is the key to long-term digestive health and symptom relief. Ultimately, understanding your body’s unique responses to food and implementing personalized strategies are paramount for navigating the complex interplay between GERD and food intolerance. Dealing with food fear is also important for overall wellbeing.