Gastroesophageal reflux disease (GERD) is a remarkably common condition affecting millions worldwide. It’s characterized by persistent heartburn, regurgitation, and discomfort after eating. While many associate GERD primarily with chest pain and digestive issues, its effects can sometimes extend to seemingly unrelated areas of the body – like the mouth and throat. One less commonly discussed symptom associated with GERD is a swollen uvula, also known as uvulitis. This article will explore the connection between GERD and a swollen uvula, helping you understand when this symptom warrants attention and what steps you can take to manage it effectively. Recognizing the subtle signs and understanding potential complications are crucial for maintaining overall health and well-being.
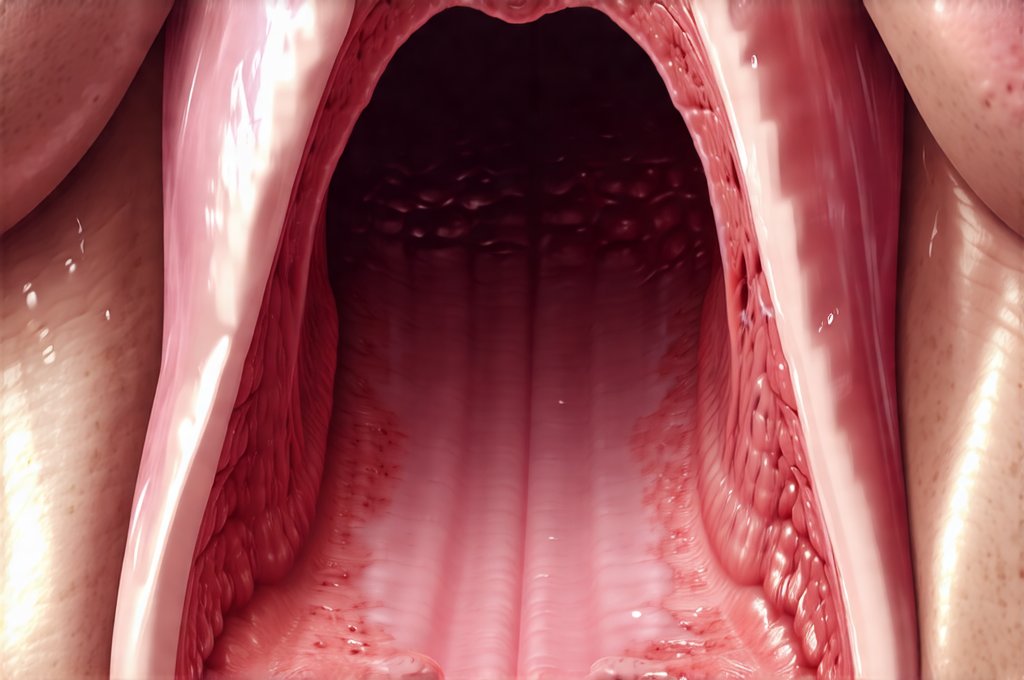
The uvula is that small, teardrop-shaped piece of tissue hanging down from the soft palate at the back of your throat. It plays a minor role in speech and swallowing, helping to prevent food from going up into your nasal passages. While typically unassuming, it’s surprisingly sensitive and can become inflamed or swollen due to various factors, ranging from infections and allergies to, importantly, acid reflux. A swollen uvula, particularly when linked to GERD, isn’t just a matter of discomfort; it signifies that stomach acid is irritating the delicate tissues in your upper digestive tract – and potentially impacting your breathing. Understanding this link allows for more informed self-assessment and timely medical consultation.
The Connection Between GERD and Uvulitis
The primary way GERD contributes to a swollen uvula is through laryngopharyngeal reflux (LPR), sometimes called silent reflux. Unlike typical GERD which presents with noticeable heartburn, LPR often lacks those classic symptoms. Instead, stomach acid creeps up the esophagus, bypassing the lower esophageal sphincter and reaching the larynx (voice box) and pharynx (throat). This acidic exposure directly irritates the uvula, causing inflammation and swelling. The irritation can be chronic and insidious, leading to persistent discomfort or a feeling of something being stuck in your throat.
This process differs from typical heartburn because the esophagus doesn’t always register the acid as strongly, resulting in fewer obvious symptoms in the chest. This makes LPR more challenging to diagnose without specific testing. The uvula’s vulnerability stems from its location and delicate tissue composition. It’s constantly exposed to everything you swallow – food, liquids, and unfortunately, if reflux is present, stomach acid. Over time, repeated exposure can lead to chronic inflammation and swelling, even with relatively mild GERD symptoms elsewhere.
It’s important to note that LPR isn’t always a direct consequence of severe GERD. Some individuals experience LPR even with minimal or no classic heartburn, suggesting individual sensitivities and variations in esophageal function. Factors like obesity, smoking, certain foods (chocolate, caffeine, alcohol), and large meals can all exacerbate reflux and increase the risk of uvulitis.
Identifying Uvulitis & When to Seek Medical Attention
Recognizing a swollen uvula is key to understanding when GERD might be playing a role – or if something else entirely is going on. Initial symptoms often include a feeling of fullness in the throat, difficulty swallowing (dysphagia), and changes in voice quality – perhaps hoarseness or a “froggy” sound. A visible swelling at the back of the mouth may also be noticeable when looking in a mirror. It’s easy to mistake these symptoms for a cold or allergies, which is why it’s vital to consider other contributing factors like heartburn or acid reflux.
However, some situations require immediate medical attention. If you experience any of the following alongside a swollen uvula, seek emergency care: – Difficulty breathing – Severe pain that makes swallowing impossible – Choking sensation – feeling as if your airway is blocked – High fever (over 101°F) These symptoms could indicate a more serious condition like epiglottitis or angioedema, which are unrelated to GERD and require immediate intervention.
Beyond these emergencies, consult a doctor if the swelling persists for more than a few days, doesn’t improve with over-the-counter remedies, or is accompanied by other concerning symptoms like blood in your saliva or significant pain. A healthcare professional can determine the underlying cause of the uvulitis and recommend appropriate treatment. If you are concerned about routine vomiting that seems unusual, it’s best to consult a doctor.
Diagnosing GERD-Related Uvulitis
Diagnosing the link between GERD and a swollen uvula often requires a multi-faceted approach, as LPR is frequently “silent.” Traditional GERD tests like endoscopy (examining the esophagus with a camera) may not always reveal abnormalities in cases of LPR. Here are some common diagnostic methods: 1. Medical History & Symptom Evaluation: Your doctor will ask detailed questions about your symptoms, dietary habits, and medical history to assess the likelihood of GERD or LPR. Pay close attention to when the swelling occurs – is it after meals, at night, or with certain foods? 2. Laryngoscopy: A laryngologist (ear, nose, and throat specialist) can perform a laryngoscopy to visually inspect your larynx and pharynx for signs of acid reflux irritation. This may involve using a flexible scope inserted through the nose. 3. pH Monitoring: This test measures the amount of acid in your esophagus over a period of time – typically 24 hours. It’s considered the gold standard for diagnosing LPR, even if typical GERD symptoms are absent. There are two main types: – Ambulatory pH monitoring (a probe is inserted through the nose) – Impedance-pH monitoring (more advanced, measures both acid and non-acid reflux).
It’s important to remember that diagnosis isn’t always straightforward. The doctor may need to rule out other causes of uvulitis, such as infections (strep throat, tonsillitis), allergies, or trauma. Sometimes, a trial period of acid suppression medication is used to see if the symptoms improve, which can help confirm LPR as the cause.
Managing GERD and Reducing Uvulitis Symptoms
Managing GERD effectively is crucial for minimizing uvulitis episodes. This often involves lifestyle modifications and, in some cases, medication. Here are some helpful strategies: – Dietary Changes: Avoid trigger foods such as chocolate, caffeine, alcohol, spicy foods, fatty foods, and acidic foods (citrus fruits, tomatoes). Eat smaller, more frequent meals rather than large ones. – Lifestyle Adjustments: Elevate the head of your bed by 6-8 inches to help prevent acid reflux at night. Avoid eating within 2-3 hours of bedtime. Quit smoking and limit alcohol consumption. Maintain a healthy weight. – Over-the-Counter Remedies: Antacids can provide temporary relief from heartburn, but they don’t address the underlying cause of GERD. H2 blockers (like famotidine) reduce acid production and may be helpful for mild symptoms.
For more severe or persistent GERD, a doctor might prescribe proton pump inhibitors (PPIs), which are stronger medications that significantly reduce stomach acid production. PPIs can be highly effective in managing LPR and reducing uvulitis symptoms but should only be used under medical supervision due to potential long-term side effects. It’s vital to work closely with your doctor to determine the appropriate treatment plan for your specific needs. If you suspect a food intolerance, consider when to try an elimination diet under medical guidance.
Beyond GERD: Other Causes of Swollen Uvula
While GERD is a common culprit, it’s essential to consider other possible causes of uvulitis. Infections like strep throat or tonsillitis can cause significant inflammation and swelling. Allergic reactions – particularly food allergies or environmental allergens – can also lead to uvulitis. Trauma from intubation (during surgery) or accidental injury can directly damage the uvula, causing swelling.
Less common causes include hereditary angioedema (a genetic condition that causes episodes of swelling), and certain autoimmune diseases. If GERD treatment doesn’t alleviate your symptoms, or if you suspect another cause, a thorough medical evaluation is necessary to identify the underlying problem and receive appropriate treatment. Don’t self-diagnose; professional guidance is crucial for ensuring accurate diagnosis and effective management. In some cases, recognizing the signs of liver failure may be important when considering alternative diagnoses. If you have concerns about digestive health, understanding colon polyps: what they are, can also be helpful. A blocked intestine might present similarly, so knowing symptoms of intestinal obstruction is worthwhile. Finally, in situations where pain is severe and sudden, remember to consider acute appendicitis as a possibility.